Committed to Providing Expertise & Quality in Vascular Care
The Vascular & Interventional Centre has a team of quality vascular surgeons, well-versed in endovascular and surgery treatments for all vascular-related diseases. Our team of specialist doctors and staff strive to provide patients with holistic care in a fully integrated clinic and Day Surgery Centre for a wide variety of vascular conditions.

Understand Your Medical Conditions & Choose The Most Suitable Treatment Options
Varicose & Spider Veins
Varicose veins are swollen and enlarged blood vessels that may cause pain and discomfort to those who have it.
Read MorePeripheral Arterial Disease
Peripheral arterial disease (PAD) is the narrowing of arteries that supply blood to the limbs caused by cholesterol & calcium deposits.
Read MoreDeep Vein Thrombosis
Deep vein thrombosis (DVT) is a condition in which blood clots form spontaneously in the deep veins of the lower or upper limbs.
Read MoreAortic Aneurysm
An Aortic Aneurysm (AA) develops when the wall of the aorta weakens and begins to bulge outwards like a balloon.
Read MoreBrain Aneurysm
Brain aneurysm is the bulging or ballooning of a blood vessel supplying the brain. Those aged 40-60 years are most likely to be affected.
Read MoreCarotid Arterial Disease
Carotid Artery Disease (CAD) occurs when one or both of the two main neck arteries “harden” and get clogged with plaque deposits.
Read MoreVascular Malformations
A vascular malformation is an abnormal growth of the arteries, veins and/or lymphatic vessels that can occur anywhere in the body.
Read MoreLymphoedema
Lymphoedema is swelling which affects the limbs due to failure of the vessels responsible for transporting the lymph.
Read MoreScrotal Pain (Varicocele)
A varicocele is a condition of tangled dilated veins within the scrotum where the valves in the testicular veins fail, blood flows backwards and pools, causing painful congestion and swelling.
Read MoreErectile Dysfunction
Erectile dysfunction is the inability to get or keep an erection and venous leak is responsible for over 80% of erectile dysfunction.
Read MoreEnlarged Prostate
Benign prostatic hyperplasia (BPH) is an enlargement of the prostate gland where the enlarged prostate compresses on the urine channel and this affects the flow and passage of urine.
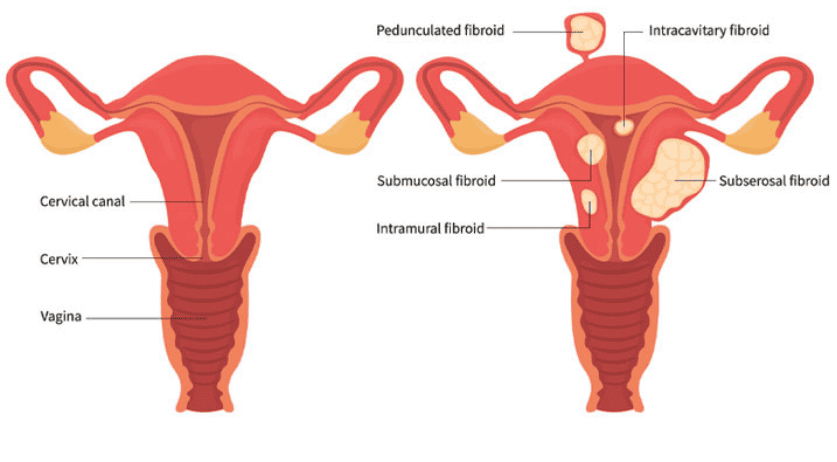
Read MorePelvic Congestion Syndrome
Pelvic Congestion Syndrome is a chronic condition that affects women and is caused by varicose veins in the lower abdomen or pelvis.
Read MorePain Management
Interventional pain management involves minimally invasive techniques specifically designed to relieve or reduce pain.
Read MoreKidney Dialysis Access
Dialysis access management helps kidney dialysis patients care for their accesses and treats dysfunctional accesses with minimally invasive procedures.
Read MoreInterventional Cancer Treatments
Interventional oncology procedures include biopsies, minimally invasive treatments of cancer.
Read MoreMake An Appointment
Our Cases & Patient Stories We Create Beautiful Smiles



Committed to Providing Expertise & Quality in Vascular Care
The Vascular and Interventional Centre (VIC) was established in March 2015 as a Singapore-based private practice dedicated to providing comprehensive care and management of conditions relating to the vascular, circulatory and lymphatic systems. More recently, VIC has expanded its portfolio to develop expertise in other aspects of interventional work including Interventional Oncology, Interventional Pain Management , Interventional Gynaecology and Lifestyle Interventional Procedures in order to provide its patients with greater holistic care.
With the latest addition of our VIC Day Surgery Centre @ Novena Specialist Center in April 2020, we have developed a one of its kind Centre in Singapore where our Specialists work as a collaborative multi-speciality team to offer patients seamless care from consultation and diagnosis to procedure and recovery at one location.
- Our Own Day Surgery Facility
- Work with Major Hospitals
- Work with Major Insurance Companies
- Multiple Clinic Locations
40+ Years
Clinical Experience
Certified Specialist
Our Specialists
Dr Benjamin Chua & Dr Chen Min Qi

Dr Benjamin Chua
Medical Director Senior Consultant Vascular Surgeon
Dr Chen Min Qi
Consultant Vascular and Endovascular SurgeonReal Review From Our Real Customer
Lorem ipsum dolor sit amet consectetur adipiscing elit sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.

Sarah Taylor
DeveloperLorem ipsum dolor sit amet consectetur adipiscing elit sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.

Aiken Ward
DesignerLorem ipsum dolor sit amet consectetur adipiscing elit sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.

Eachann Jhon
FounderLorem ipsum dolor sit amet consectetur adipiscing elit sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.