Introduction to Varicoceles
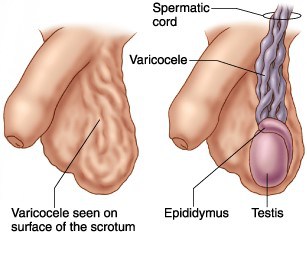
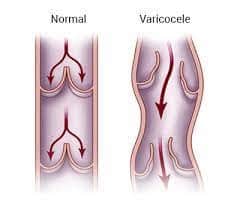
A varicocele is characterised by a cluster of enlarged veins within the scrotum. These veins play a crucial role in the blood circulation of the testicles, supporting their essential functions. The testes (testicles) are located in the scrotum, which is a pouch of skin behind the penis. Similar to varicose veins observed in the legs, if the valves in the testicular veins malfunction, blood can flow in the opposite direction, leading to pooling and stagnation in the testes. Consequently, this condition causes painful congestion and swelling.
(https://www.tsmp.com.au/blog/varicocele-ultrasound.html)
Varicoceles, for the most part, are often asymptomatic, causing no noticeable pain or discomfort. However, in certain instances, some individuals may experience intermittent testicular pain. Beyond the potential for discomfort, varicoceles can also have more significant implications, particularly in relation to fertility. For some people, this condition might lead to infertility, as it can affect sperm production and quality. Nevertheless, it’s essential to note that not all varicoceles automatically result in fertility issues.
Causes and Symptoms of Varicocele
Varicoceles are estimated to affect up to 20% of males worldwide, and it can be easily treated using both conventional and minimally invasive procedures. Medical professionals and healthcare providers are unsure about the exact cause of varicoceles. Some speculate that they could be caused by a malfunctioning “switch” (valve) in specific spermatic cord veins. Testicles are fixed in place by a band of tissues called the spermatic cord and the testicles’ blood is returned to the body through veins that accompany the spermatic cord. The valve functions something like an “on/off” switch. It features two structures that resemble flaps that aid in blood flow back towards your heart. Blood may accumulate inside the veins in your testicles when a valve doesn’t function as it should. As veins enlarge throughout time, which may cause potential complications in these organs.
(https://www.fatihatugmd.com/varicocele)
At any age, anyone with testicles is susceptible to varicoceles. Varicoceles are thought to be congenital, which means that this condition is present at birth. When an individual undergoes puberty, the blood flow to the genitals increases. Many people first become aware of their varicocele in their teenage years and in some rare cases, varicocele may occasionally stop your testicles from developing normally.
While many people with varicocele may stay asymptomatic, showing no overt symptoms or discomfort, in other instances the condition can result in a number of symptoms such as:
- Discomfort in the scrotum and testicles, which can range from sharp to dull pain
- Heightened pain while standing or engaging in physical activities, particularly during extended durations.
- Alleviation of pain when lying down.
- Presence of a lump or swelling in one of the testicles.
- Noticeable enlargement or twisting of veins in the scrotum, often resembling a “bag of worms”.
- Possible testicular atrophy, indicating reduced size or development of the testicles.
While certain individuals may remain pain-free, varicoceles can significantly contribute to reduced sperm production and diminished sperm quality. As a consequence, approximately 40% of men facing difficulties in conceiving their first child may ultimately experience infertility.
Diagnosis and Treatments for Varicocele
To diagnose a varicocele, your healthcare provider will perform a visual inspection and palpation of the scrotum, both while lying down and standing up. During the examination, you may be asked to perform the Valsalva maneuver, where you take a deep breath, hold it, and bear down, which aids in examining the varicocele more effectively.
Fortunately, if you have a varicocele, there is often no need for excessive concern. Diagnosis is usually straightforward, and many cases do not require treatment unless they cause noticeable and obstructive symptoms. In some cases, varicoceles are typically detected through self-examination of the scrotum or during routine medical check-ups. They are recognizable by their appearance and can be assessed by feeling the size of the spermatic cord and testicles during physical examinations. If any issues are detected during these examinations, your vascular surgeon may opt for an ultrasound test to identify veins wider than 3 millimetres, which could indicate the presence of a varicocele.
“Subclinical” varicoceles, which are detected on ultrasound, are generally not considered to be clinically significant since they rarely cause testicular issues or discomfort. In some cases, ultrasound might be used when a physical examination is challenging due to anatomical factors or when other findings warrant further investigation. While large varicoceles may be visible to the naked eye or cause a distinct “bag of worms” sensation in the scrotum, most varicoceles are detected during a vascular surgeon’s examination. Thus, the most reliable way to identify a varicocele is through a thorough physical examination by a vascular surgeon.
Treatment Options for Varicocele
1.Traditional Surgery
A varicocelectomy is a surgical procedure performed in a hospital setting to treat varicoceles. The surgery involves blocking the blood flow in the veins of the spermatic cord and is conducted under general anesthesia. There are two methods of performing a varicocelectomy: microscopic and laparoscopic. In the microscopic varicocelectomy, a urologist clamps or ties all small veins through a 1cm incision above the scrotum, while in the laparoscopic varicocelectomy, thin tubes are inserted into the abdomen to ligate the veins. Conventional treatment is usually open or laparoscopic surgery. Both procedures take different durations to complete but generally have a similar healing time (several weeks) and pain level.
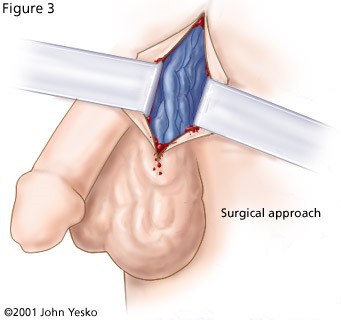
(https://varicoceles.com/treatment-options/)
While varicocelectomy is generally considered a safe procedure, like any surgery, it carries some potential risks and complications. These complications may include:
- Varicocele persistence or recurrence: In some cases, the varicocele might not be entirely resolved by surgery, leading to its persistence or recurrence. This may be due to incomplete ligations of the affected veins or the development of new abnormal veins over time.
- Hydrocele: Fluid accumulation around the testicle, known as a hydrocele, is another possible complication. It may occur as a result of the surgical procedure, leading to swelling and discomfort.
- Injury to the testicular artery: While performing the surgery, there is a slight risk of inadvertent injury to the testicular artery, which supplies blood to the testicles. However, such injuries are exceedingly rare and typically managed promptly by the surgical team.
It is essential for patients to discuss these potential risks with their healthcare providers before undergoing a varicocelectomy. This will allow them to make an informed decision and to be aware of the steps taken to minimize the occurrence of complications during the surgical procedure.
2.Percutaneous embolisation
Embolisation is a minimally invasive medical procedure used to treat varicoceles, a condition characterized by enlarged and abnormal veins within the scrotum. The procedure is typically performed by an interventional vascular surgeon. To begin the embolization, the patient is typically given a local anaesthetic to numb the area where the catheter will be inserted. Then, a small puncture is made in a vein in the upper thigh, to gain access to the blood vessels. Through this access point, a catheter is carefully threaded through the vascular system using real-time X-ray guidance called fluoroscopy.
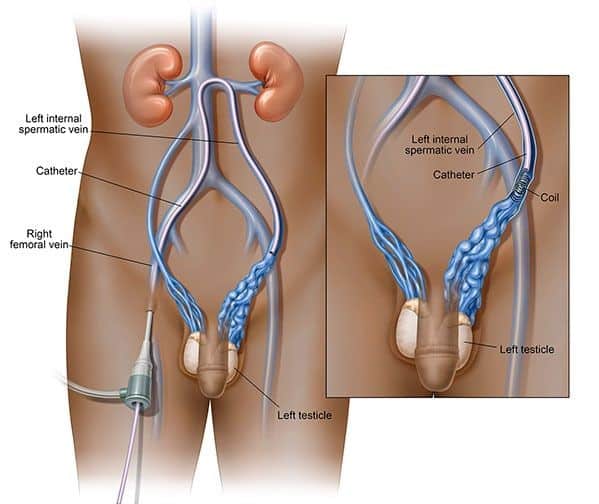
(https://www.azuravascularcare.com/medical-services/varicocele-embolization/)
The catheter is guided to the affected blood vessels that are supplying the varicocele(s). These are the veins that are responsible for the abnormal blood flow and enlargement of the veins in the scrotum. Once the catheter is in position, tiny titanium coils and an embolic agent are introduced through the catheter and into the targeted vessels. The embolic agent used in the procedure is usually small particles or special liquids that have the ability to block off the blood supply to the varicocele. This is achieved by causing clotting in the targeted veins, effectively sealing them off from the blood flow. The tiny titanium coils are used to support and stabilize the embolic agent, ensuring it remains in place and effectively blocks the abnormal veins. By blocking off the blood supply to the varicocele, embolization aims to redirect the blood flow through healthier veins, restoring normal circulation and reducing the size of the varicocele over time. The procedure typically takes around one to two hours to complete and is performed on an outpatient basis, meaning the patient can usually go home the same day.
The Benefits of Embolisation
Vascular & Interventional Centre offers embolisation, a minimally invasive varicocele treatment. Embolisation has advantages over open or laparoscopic surgery:
- Embolisation is less intrusive than surgery. It reduces infection and scarring with a small puncture. Less post-operative pain and discomfort speeds recovery and return to normal activity.
- Local Anaesthesia: Unlike surgery, embolisation is done under local anaesthesia. This improves procedure safety and comfort.
- Embolization’s less-invasive nature speeds healing. Unlike conventional surgery, most patients can go home the same day and resume normal activities within a few days.
- Embolisation is equally effective as surgery in treating varicoceles. The technique reduces varicocele size and pain by diverting blood flow and closing aberrant veins.
- Outpatient Procedure: Patients can go home after embolisation. This minimises hospital stays and expenditures, making therapy convenient.
- Lower Risk of Complications: Because embolisation is less invasive, it has a lower risk of infection, bleeding, and tissue damage than conventional surgery.

(https://www.sciencedirect.com/science/article/pii/S2211568418301499)
Compared to varicocele surgery, embolisation is safe, effective, and patient-friendly. We use comprehensive techniques to give our patients the optimal results to address symptoms. Percutaneous embolization is a suitable option for patients who meet specific eligibility criteria. Individuals diagnosed with varicocele and experiencing aggravated symptoms of testicular pain are among the suitable candidates for this procedure. Additionally, patients who prefer to avoid invasive surgery may also find percutaneous embolization to be a viable and less invasive alternative for addressing their varicocele. By considering these factors, healthcare providers can determine whether percutaneous embolization is the appropriate treatment choice for eligible patients seeking relief from varicocele-related symptoms.
Preparing for Varicocele Treatment
Before the treatment, it is very important to tell your doctor about all the medicines you are taking, including herbal supplements, and about any allergies you have, especially to local anaesthetic, general anaesthesia, or contrast materials. Before the surgery, your doctor may tell you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), or blood thinners. You will be given clear advice on how to get ready, including any changes to your regular medication schedule that may be needed. If you will be given a sedative during the procedure, your doctor may tell you not to eat or drink for four to eight hours before the operation. In these situations, you may need someone to go with you and drive you home afterwards. You will be given a gown to wear during the process.
What to Expect During Varicocele Treatment
During the procedure, a member of the staff will cleanse the skin above the catheter insertion point and apply a local anaesthetic to minimize any discomfort. Intravenous sedation is typically given to ensure you feel relaxed and comfortable throughout the procedure, and you will not usually feel the catheter during the process. Devices will be attached to monitor your heart rate and blood pressure.
When the nurse inserts the needle for the IV line and injects the local anaesthetic, you may feel a slight pinch, mainly at the skin incision site. The doctor will numb this area using a local anaesthetic, ensuring you experience minimal discomfort. While the doctor inserts the catheter into the vein or artery, you may feel some pressure, but serious discomfort is unlikely. If sedation is used during the procedure, you will feel relaxed and may become sleepy, with the depth of sedation determining whether you remain awake or not.
As the contrast material passes through your body, you may feel a brief warm sensation, but it will quickly pass. After the procedure, you will stay in the recovery room until you are fully awake and ready to return home. In most cases, you should be able to resume your normal activities within a few days after the procedure. However, due to the intentional clotting of blood in the treated vein, localized scrotal discomfort might be experienced for up to a week following the procedure.
Final Words
Consulting with a vascular surgeon is crucial when dealing with varicocele, a condition characterized by enlarged veins in the scrotum. While many cases are asymptomatic, varicoceles can cause testicular pain and even lead to infertility. Vascular surgeons possess specialized expertise in diagnosing and treating varicoceles, offering a thorough evaluation and personalized treatment plan. Traditional surgical options like varicocelectomy are available, but percutaneous embolization provides a less invasive and equally effective alternative. Embolization involves using tiny titanium coils and an embolic agent to block abnormal veins’ blood supply, restoring normal circulation. Compared to surgery, embolization offers advantages such as less scarring, reduced post-operative pain, and faster recovery.
FAQ:
Varicocele is a condition characterized by enlarged veins in the scrotum, potentially causing pain and swelling due to blood flow issues. While many cases are asymptomatic, varicoceles can impact fertility, making it important to consult a vascular surgeon for a thorough evaluation and personalized treatment options.
Varicoceles can lead to fertility issues in some individuals due to their potential impact on sperm production and quality. However, not all varicoceles automatically result in fertility problems.
Varicoceles can be asymptomatic in many individuals, but in others, they may cause discomfort in the scrotum and testicles, pain during physical activities, swelling, twisted veins, and possible testicular atrophy. Additionally, varicoceles can lead to reduced sperm production and quality, potentially causing infertility in around 40% of men facing difficulties conceiving their first child.
Varicoceles are not preventable because they are congenital, meaning they are present from birth and result from abnormalities in the veins’ structure and valves in the scrotum. As a congenital condition, there are no preventive measures to avoid its development.
Diagnosing a varicocele involves a visual inspection and palpation of the scrotum while lying down and standing up. The Valsalva manoeuvre may be used to aid in the examination. If detected, varicoceles usually don’t require immediate treatment unless they cause noticeable symptoms; they can often be identified through physical examinations by a vascular surgeon, but ultrasound may be used for confirmation or when physical examination is challenging.
Varicoceles can be treated through traditional surgery known as varicocelectomy, performed in a hospital setting under general anaesthesia. This surgical procedure involves blocking the blood flow in the veins of the spermatic cord through either microscopic or laparoscopic methods. However, varicocelectomy carries some potential risks, including varicocele persistence or recurrence, hydrocele formation, and rare injury to the testicular artery.
An alternative, less invasive option is percutaneous embolisation, performed by an interventional vascular surgeon. This procedure uses a catheter to block the abnormal veins with tiny titanium coils and an embolic agent, redirecting blood flow and reducing the varicocele’s size. Embolisation is typically done on an outpatient basis, taking around one to two hours, and offers advantages such as shorter recovery time, minimal scarring, and lower risk of complications.
Yes, varicoceles can negatively impact sperm production and quality. Around 40% of men facing difficulties conceiving their first child may have varicoceles.
Inform your doctor about current medications and allergies
Avoid aspirin, NSAIDs, or blood thinners as instructed
Follow fasting guidelines if sedation is required
Arrange for someone to accompany you if needed
During the varicocele treatment, you will be given a local anesthetic and possibly IV sedation for comfort. A catheter or surgical instruments will be used to address the varicocele, with monitoring of vital signs throughout the procedure.
Vascular & Interventional Centre is here to address your vascular needs. You can explore our website for more resources about conditions and our treatments. You can also visit our Facebook page for additional information.
References
[1] https://my.clevelandclinic.org/health/treatments/24234-varicocelectomy
[2] https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/varicocele-embolization
[3] https://www.mayoclinic.org/diseases-conditions/varicocele/diagnosis-treatment/drc-20378772
[4] https://www.radiologyinfo.org/en/info/varicocele

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- varicocele causes
- varicocele clinic Singapore
- varicocele complications
- varicocele diagnosis
- varicocele fertility impact
- varicocele health advice
- varicocele laser treatment
- varicocele management Singapore
- varicocele minimally invasive
- varicocele outpatient care
- varicocele pain relief
- varicocele patient education
- varicocele recovery
- varicocele specialist Singapore
- varicocele surgery Singapore
- varicocele symptoms
- varicocele treatment cost Singapore
- varicocele treatment singapore
- varicocele vascular health
- varicocele vein treatment
