An Overview of Aortic Aneurysm
The aorta plays a critical role in the circulatory system as the largest and main artery in the body. Its primary function is to carry oxygenated blood away from the heart and distribute it to various parts throughout the body like the liver, stomach, intestines, and kidneys. The aorta originates directly from the heart’s left ventricle, the chamber responsible for pumping oxygen-rich blood into the aorta. This blood is then propelled through the aorta’s various segments to supply the entire body with the necessary nutrients and oxygen for proper functioning.
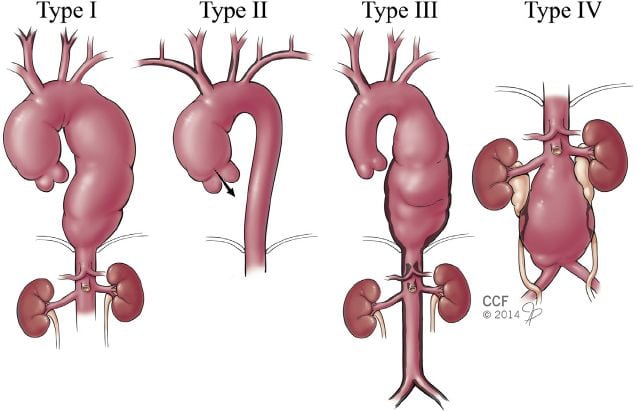
An aortic aneurysm occurs when a weakened area of the aortic wall becomes dilated or ballooned, potentially causing the vessel to expand beyond its normal size. The pressure of the blood flowing through the aorta can push against the weakened wall, causing it to bulge outwards. This condition is particularly dangerous because the stretched and weakened wall is more susceptible to rupture, leading to internal bleeding. Aneurysms can develop in various segments of the aorta, leading to different types:
(https://www.researchgate.net/publication/265128530_Inflammatory_Disease_of_the_Aorta_Patterns_and_Classification_of_Giant_Cell_Aortitis_Takayasu%27s_and_Non-Syndromic/figures?lo=1)
- Thoracic Aortic Aneurysm (TAA): Aneurysm that occurs in the chest portion of the aorta.
- Abdominal Aortic Aneurysm (AAA): Aneurysm that forms in the abdomen.
- Thoracoabdominal Aortic Aneurysm (TAAA): Aneurysm that spans both the thoracic and abdominal segments of the aorta.
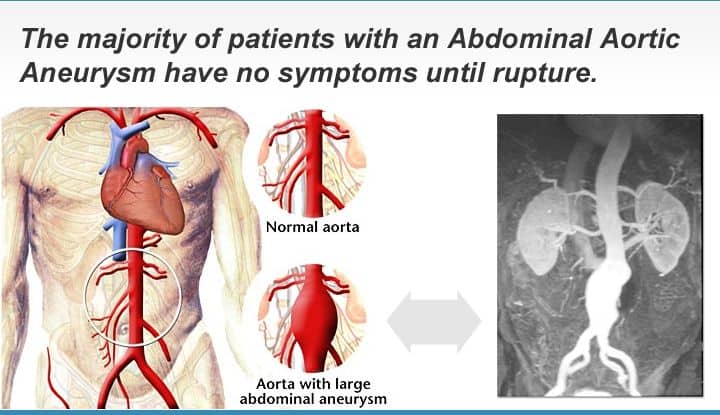
Aneurysms are particularly concerning because they can remain asymptomatic and undetected until they grow to a critical size or rupture. Small aneurysms may not pose an immediate threat, but as they enlarge, the risk of rupture increases. A ruptured aortic aneurysm is a medical emergency and can lead to severe internal bleeding, shock, and potentially death if not promptly treated through surgical intervention.
Symptoms of Aortic Aneurysms
- Severe and enduring pain in the chest, abdomen, back, or lower limbs could signal an aortic aneurysm’s presence due to pressure on nearby tissues.
- A persistent fever may indicate infection or inflammation linked to the aneurysm.
- An abdominal aortic aneurysm can create a pulsating sensation in the abdomen due to the aneurysmal wall’s expansion with each heartbeat.
- Reduced blood flow from an aneurysm could lead to gangrene or dark, discolored patches on the toes, which might indicate tissue damage.
Remember, these symptoms may vary from person to person, and some aneurysms might not cause any noticeable symptoms until they become more serious. If you suspect an aortic aneurysm, seek medical attention from a vascular surgeon for proper evaluation and guidance even if there are no symptoms.
(https://www.preventionhealthscreenings.com/portfolio-item/abdominal-aortic-aneurysm-screening/)
Common Causes and Risk Factors of Aortic Aneurysms
- Chronic Smokers – Chronic smokers are strongly advised to consult a vascular surgeon due to their heightened risk of aortic aneurysm development linked to the weakening effects of tobacco.
- Older than 65 Years, Predominantly Males – Those aged over 65, particularly males, should seek a vascular surgeon’s consultation considering their increased vulnerability to aortic aneurysms.
- Long-Term Hypertension and/or Heart Disease – Individuals with prolonged hypertension and/or heart disease should consult a vascular surgeon due to their elevated risk of aortic aneurysms from potential strain on blood vessel walls.
- Congenital Soft Tissue Diseases – Those with congenital conditions like Marfan syndrome, Ehlers-Danlos syndrome, or Loeys-Dietz syndrome should consult a vascular surgeon owing to genetic factors that heighten susceptibility to aortic aneurysms.
- Strong Family History of Aortic Aneurysms and Dissections – Individuals with a strong family history of aortic aneurysms and dissections should consult a vascular surgeon to address the hereditary predisposition and consider appropriate screening measures.
Individuals with these risk factors should consider consulting a vascular surgeon for aortic aneurysm assessment and guidance. Early detection and management can help mitigate the risks associated with aneurysm development, potentially preventing complications such as rupture and ensuring overall cardiovascular health.
Diagnosis And Tests for Aortic Aneurysm
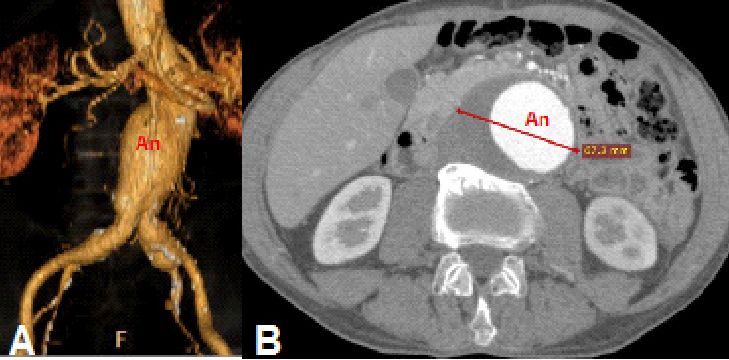
Aortic aneurysms are diagnosed through clinical examination, where a throbbing abdominal mass can be felt, and confirmed with imaging tests such as ultrasound scans or CT scans. Often discovered incidentally during routine checkups, these aneurysms may develop without symptoms. For individuals at high risk or exhibiting symptoms, imaging tests like CT scans create detailed cross-sectional images, while ultrasounds use sound waves for non-invasive visualization of the aorta, aiding accurate diagnosis and assessment of the aneurysm’s size, properties, and characteristics.
(https://www.researchgate.net/publication/328756585_Use_of_3D_Printing_in_Preoperative_Planning_and_Training_for_Aortic_Endovascular_Repair_and_Aortic_Valve_Disease/figures?lo=1)
Treatment Options for Aortic Aneurysm
Traditional Surgical Repair
Open Surgical Repair is a conventional and traditional approach for treating aortic aneurysms. In this method, long incisions are made in the chest/abdominal wall to directly access the aneurysm and repair it. While this method is robust, it carries substantial risks of complications and even death due to its invasive nature. It’s typically recommended for younger patients with lower surgical risk. Following surgery, patients often require intensive care unit (ICU) monitoring for about a week, and the overall recovery period can range from one month to six weeks. This method’s longer recovery time and higher risks have led to its limited use, especially in comparison to newer, less invasive treatments.
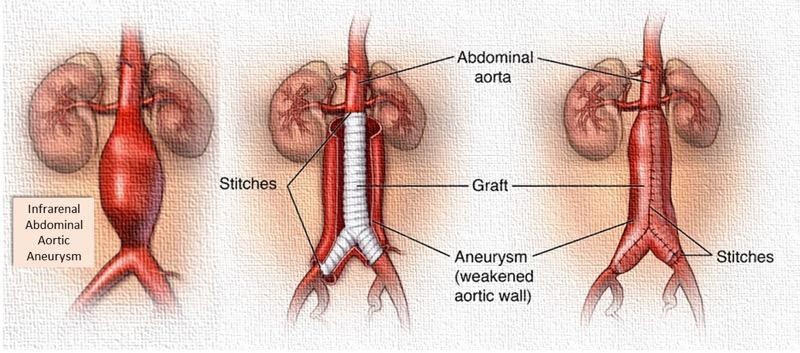
(https://www.vascularhealth.gr/en/vascular-procedures/abdominal-aortic-aneurysm-open-repair)
Minimally Invasive Repair
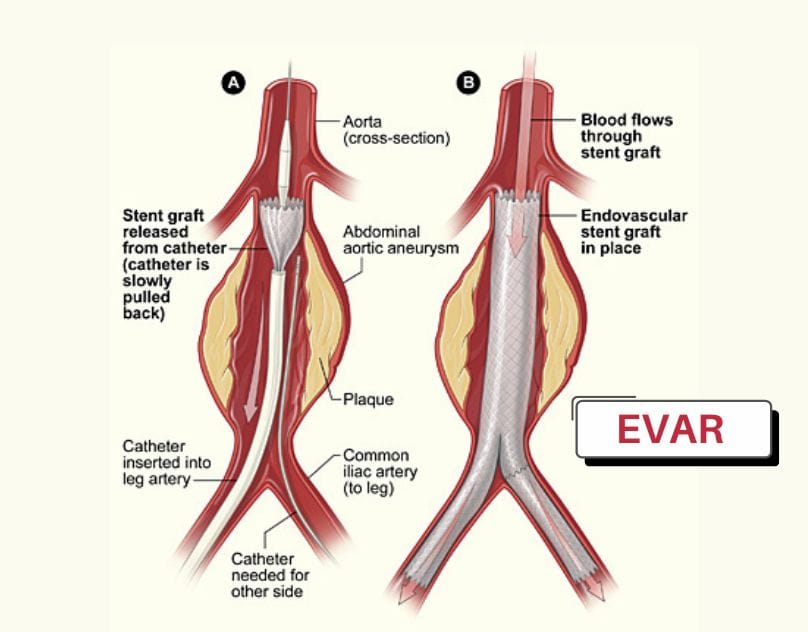
Minimally Invasive Repair offers a modern approach to treating aortic aneurysms through a less invasive procedure known as EndoVascular Aortic Repair (EVAR). This method uses special stents designed to hold the vessel open. The procedure involves making small (approximately 1cm) incisions in the groin to access the femoral arteries in the leg. Through these incisions, the stent-grafts are inserted and guided to the site of the aneurysm using X-ray guidance (fluoroscopy). The stent-grafts are positioned to reline the vessel and exclude the aneurysm from the arterial blood pressure circulation.
(https://www.drameetoswal.com/aortic-stent-graft/)
The Advantages of EndoVascular Aortic Repair (EVAR)
EVAR is particularly suitable for older patients or those with multiple medical conditions that result in additional surgical risks. Its minimally invasive nature allows for the procedure to be performed under local anaesthesia and mild sedation. Unlike open surgical repair, EVAR patients typically don’t require an extended ICU stay. They are often up and moving within 8 hours after the procedure and can be discharged from the hospital as early as 48 hours post-surgery. In some cases, younger and healthier patients can even be discharged on the same day as the procedure, offering a quicker recovery compared to more invasive approaches.
Prognosis for People with an Aortic Aneurysm
By closely monitoring and providing appropriate medical interventions, your vascular surgeon can assist you in effectively handling an aortic aneurysm. The aim is to detect and address the aneurysm before it reaches a point of rupture. In the event of an aortic aneurysm rupture, it is crucial to promptly seek medical attention. Without timely intervention, a ruptured aortic aneurysm can have fatal consequences.
FAQs:
A vascular surgeon can assist in treating an aortic aneurysm by providing specialized care and interventions. They can monitor the aneurysm’s progression and recommend suitable treatment options based on the patient’s condition and lifestyle. The goal is to prevent aneurysm rupture, which could lead to life-threatening internal bleeding.
An aortic aneurysm is a medical condition where a weakened area of the aortic wall becomes dilated or ballooned, causing the blood vessel to expand beyond its normal size. This can lead to dangerous consequences, as the stretched and weakened wall becomes more susceptible to rupture, potentially resulting in severe internal bleeding.
Symptoms of an aortic aneurysm include severe and enduring pain in the chest, abdomen, back, or lower limbs, persistent fever, pulsating sensation in the abdomen, and reduced blood flow leading to potential tissue damage or gangrene in the toes. Unfortunately, many of the symptoms manifest late in the disease when potentially life-threatening rupture has occurred. It is imperative that individuals with risk factors for developing an aortic aneurysm, be screened for the presence of one even if there are no symptoms.
Aortic aneurysms are diagnosed through clinical examination, and imaging tests like ultrasound scans or CT scans, with incidental discovery during checkups, enabling accurate assessment of the aneurysm’s characteristics and size.
Traditional Surgical Repair involves Open Surgical Repair, a conventional approach for treating aortic aneurysms through chest wall incisions to access and repair the aneurysm, but its invasiveness brings substantial risks and a longer recovery period, especially for younger patients; Minimally Invasive Repair, on the other hand, offers a modern alternative using EndoVascular Aortic Repair (EVAR), a less invasive procedure utilizing special stents inserted through small incisions in the groin to exclude the aneurysm from blood pressure circulation under X-ray guidance.
References
- https://www.sgvascularctr.com/service/aortic-aneurysm/
- https://my.clevelandclinic.org/health/diseases/16742-aorta-aortic-aneurysm
- https://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/symptoms-causes/syc-20350688

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- Aortic aneurysm
