What are Varicose Veins?
Varicose veins are a very common condition with up to half the adult population experiencing some degree of venous stigmata in their lifetime. Varicose veins are twisted superficial veins, usually found on the legs, and can be unsightly and uncomfortable but do not cause serious medical problems unless left untreated. The most prominent symptom of varicose veins is their appearance: bulging or swollen blue-green lines that protrude underneath the skin’s surface.
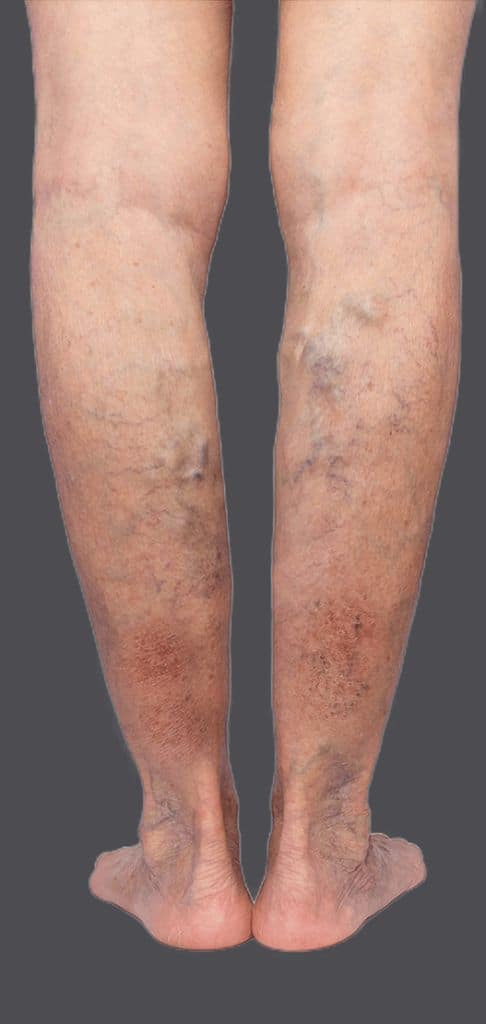
Image source: (https://australianveinclinics.com.au/venous-disease-progression/)
Other symptoms include heaviness or fatigue in the limbs, muscle cramps at night, itching around the affected area(s), swelling of leg and ankles especially after standing for long periods, and discoloration (darkening) of the skin.
What Causes Varicose Veins?
Veins are thin-walled vessels that function to return blood back to the heart. The veins in the legs need to transport blood against gravity to fulfill their function and they rely on two mechanisms to achieve this:
- The contraction of the surrounding muscles (especially the calf muscles) to squeeze the veins and push the blood back to the heart.
- One-way channels called valves which allow the blood in the veins to only flow in one direction (i.e. towards the heart). These valves will close and prevent back-flow of the blood in the veins.
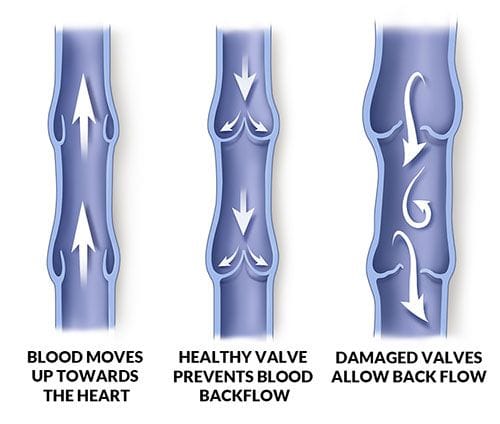
Image source: (https://austinheartvein-vascular.com/vein-disease-symptoms/)
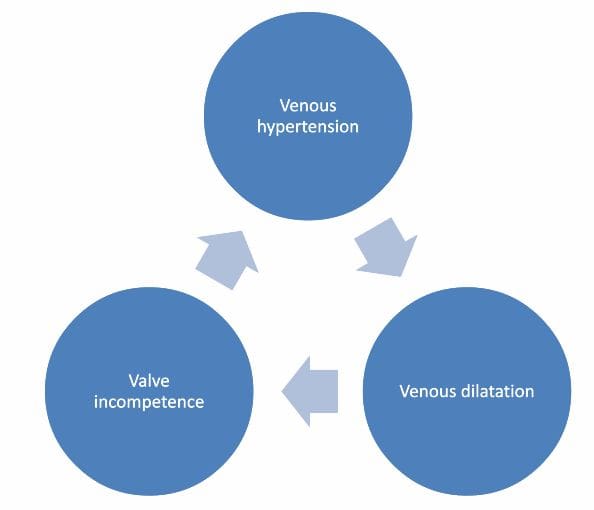
Varicose veins occur when the pressure of the blood within the vein increases (high venous pressures). This stretches the thin-walled veins causing them to swell and undergo inflammation which damages the one-way channels (valves) within the vein. As the valves get progressively damaged, they lose their function, thus allowing a back-flow of blood. This back-flow of blood contributes to increasing the venous pressure, thus perpetuating the vicious cycle of swelling, valve damage and high venous pressures.
Factors that increase the risk of developing varicose veins include:
1.Genetics – a family history of varicose veins (i.e. parents/siblings having the same condition).
2.Gender – female hormones relax the thin-walled veins allowing them to stretch and become swollen. Hormone changes with menopause (or taking birth control pills) also has a similar effect.
3.Age – The vein elasticity and the valve function usually deteriorate over time resulting in increased risk of varicose veins most commonly after the age of 40.
4.Pregnancy – The overall blood volume is increased during pregnancy and coupled with the pressure of the fetus on the pelvic vessels, causes enlargement of the leg veins.
5.Obesity – Just as with pregnancy, excessive body weight causes increased circulatory blood volume and puts pressure on the pelvic vessels resulting in varicose vein formation.
6.Sedentary lifestyle/prolonged standing – The leg veins require the surrounding muscles to contract and squeeze the blood back to the heart. The paucity of leg muscle contraction in an occupation that involves prolonged standing or a sedentary lifestyle, results in pooling of blood in the veins resulting in varicose vein formation.
What Are the Symptoms of Varicose Veins?
In the early stages of the disease (stage 1 & 2), varicose veins mainly pose a cosmetic issue with unsightly bulging bluish-green cords seen protruding just beneath the skin surface. These are especially prominent in people with fair skin color.
As the disease progresses, patients will start to experience “heaviness” or aching discomfort in the lower leg/ankles with occasional cramps in the calf muscles. In stage 3 of the disease, swelling and water retention in the legs occur.
When the leg is swollen, it becomes more difficult for oxygen and nutrients to be transmitted from the blood vessels to the skin surface. Waste products and toxins from the cells near the skin surface are also not effectively removed. This results in poor skin quality. The skin is dry and itchy and is prone to recurrent skin infections.
In stage 4 of the disease, the skin develops dark spots (pigmentation) which are unfortunately permanent, and the skin also thickens and hardens (lipodermatosclerosis). If still left untreated, the patient will eventually develop ulcers (open sores).

Image source: (https://cardiologyinstitute.co.nz/gp-info/2022/2/12/chronic-venous-insufficiency)
Other symptoms that can occur at any stage of the disease include:
- Bleeding – The bleeding from injury to varicose veins can be very massive due to the high venous pressures causing large amounts of blood loss in a short period of time. If there is bleeding from varicose veins, immediately lie down, raise the leg above the head and apply pressure to the bleeding point.
- Inflammation (thrombophlebitis) – Blood clots can occasionally occur in the superficial varicose veins due to the lack of circulation. The segment of clotted vein will undergo inflammation resulting in a warm, painful swelling felt along the length of the vein. Thrombophlebitis usually recovers with just anti-inflammatory medications.

Image source: (https://www.centerforvaricoseveins.com/blog/should-i-see-a-vein-specialist-for-superficial-thrombophlebitis)
- Deep venous thrombosis (DVT) – Anyone with varicose veins is at increased risk of clots forming in the deep veins of the leg resulting in DVT. This can occur especially during periods of prolonged immobility, and can be life-threatening if the clots dislodge and travel to the lungs. It is highly advised that anyone with varicose veins wear compression stockings if they will be sitting for a prolonged period (such as during a long-haul flight).
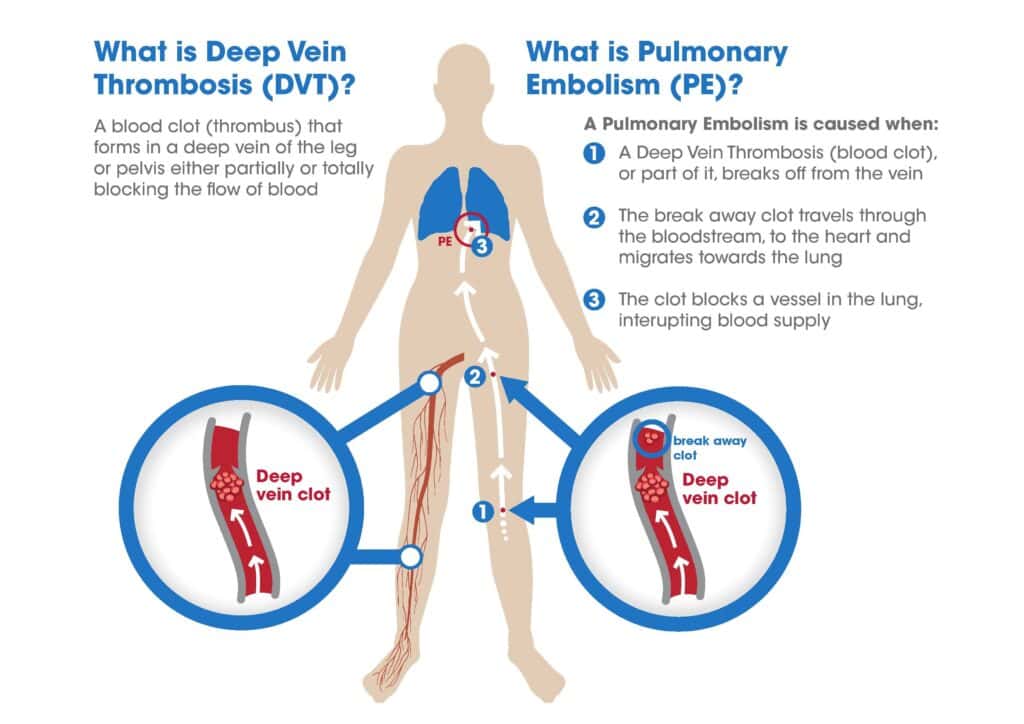
Image source: (https://www.capital-medical.com/products/dvt-pe-treatment/)
How are Varicose Veins Diagnosed (Investigations for Varicose Veins)?
A thorough work-up for varicose veins begins with a pertinent history and physical examination looking for any risk factors that may be present as well as any symptoms and complications of the disease. Please see above sections “What Causes Varicose Veins?” and “What Are the Symptoms of Varicose Veins?” for more details.
An ultrasound evaluation is next performed where the doctor/radiographer will scan at various segments along the leg veins while applying pressure to the calves. The ultrasound can detect any malfunctioning valves in the segment of vein, indicating that this segment is diseased. This is sometimes termed a venous reflux scan, as the faulty valves will produce refluxing flow as detected by the ultrasound machine.

Image source: (https://advancedheartandvein.com/do-i-need-a-leg-arterial-ultrasound/)
Occasionally a CT scan (computer tomography) may be performed to evaluate the larger veins in the abdomen and pelvis if the doctor suspects some disease there.
How are Varicose Veins Treated?
Management of varicose veins are broadly classified into surgical and non-surgical measures. Non-surgical measures are useful in preventing the onset or delaying the progression of the disease, however to remove already diseased veins, surgery will be necessary.
Non-surgical management of varicose veins include:
1.Weight reduction
Many studies show increased risk of varicose veins (venous insufficiency) in patients with a BMI of >30kg/m2. Maintaining an ideal body weight (BMI of 25 kg/m2) would greatly reduce the risk of developing varicose veins.

Image source: (https://www.freepik.com/free-photos-vectors/asian-gym/2)
2. Graduated compression stockings
Graduated compression stockings are specialized stockings (knee/thigh length) with a gradient of pressure along its length (highest pressure exerted at the feet and gradually reducing upwards). There are 3 grades of compression, with the middle grade 2 compression (20-30mmHg) recommended for varicose veins.
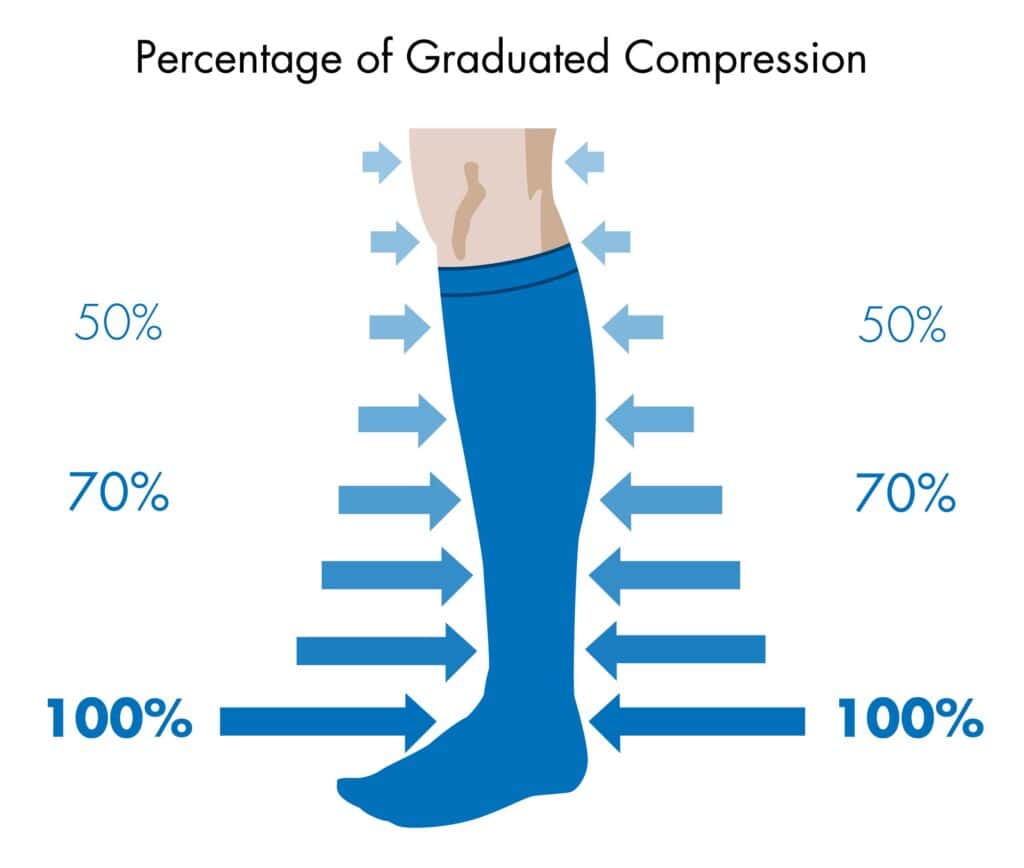
Image source: (https://healthyeye.co.za/tag/compression-stockings/)
3. Avoid prolonged sitting/standing
Many people whose occupation involves prolonged standing/sitting (i.e. continuous immobility for >1h or total immobility of >4h in a day) are at higher risk of varicose veins. These patients should be advised to wear graduated compression stockings while at work and engage in calf pump exercises or take walking breaks at regular intervals.
4. Avoid smoking/tobacco use
It is generally good advice to avoid smoking/tobacco. It will not only reduce the risk of varicose veins, but more importantly reduce the risk of stroke, heart attack and COPD.
Surgery for varicose veins depends on the size and location of the vein. Frequently, a combination of surgical modalities will be utilized to achieve optimal results.
Vein Stripping and Ligation: This is a largely outdated surgical technique that involves surgically removing the entire varicose vein via skin incisions made above and below the diseased vein. It has largely been replaced by minimally invasive surgical techniques and is only considered in very specialized cases such as in veins larger than 2cm in diameter.
Endovenous thermal ablation: This is a minimally invasive procedure in which heat energy such as radio frequency (RFA) or laser (EVLT) is used to close off the faulty veins. The device is introduced via a small 5mm incision around the level of the knee, and it has the benefit of being relatively painless with minimal downtime. Its use in the veins below the knee should be avoided if possible, as this may result in injury to the nerves (saphenous and sural nerves) which are in close proximity to the vein.
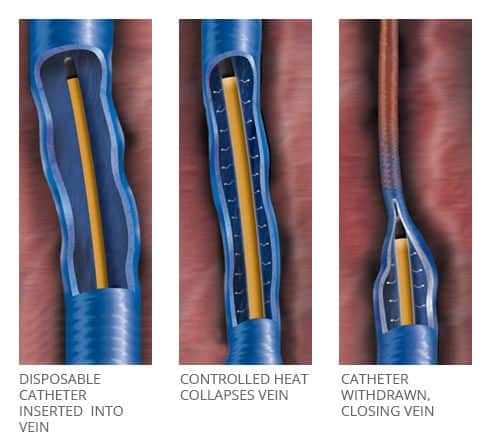
Image source: (https://www.veinhealth.com.au/radiofrequency-ablation/)
Sclerotherapy: Sclerotherapy involves injecting a chemical solution (known as a sclerosant) into the faulty veins via a needle or catheter to cause their closure. It is not as effective for veins larger than 5mm in diameter and is predominantly used to treat the smaller more tortuous veins which cannot accommodate the endovenous thermal ablation device, as well as to treat the veins below the knee to reduce the risk of nerve injury.

Image source: (https://bankersvascular.com/foam-sclerotherap/)
Cyanoacrylate (Bioadhesive) Glue Treatment: This is a relatively new method for closing off varicose veins. Just as with endovenous thermal ablation, it is minimally invasive involving only a small 5mm incision in the skin. It has the added advantage of being able to treat the vein below the knee, without risk of nerve damage, and can treat veins with diameters up to 1cm. There is a risk of allergy/inflammatory reaction to the injected glue and patients need to take a course of anti-inflammatory medications for a couple of weeks after the surgery.
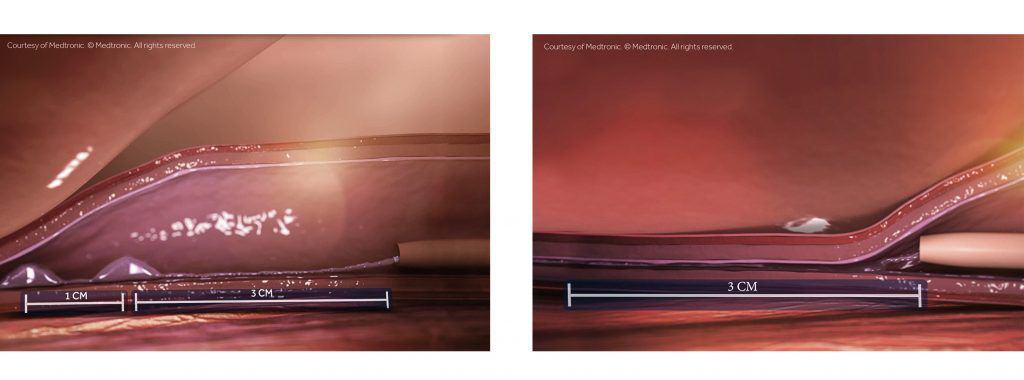
Image source: (https://frpsclinics.org/venaseal-closure-system/)
Cryo-laser ablation:This technique is effective for small 1-2mm reticular (spider) veins. Laser energy is directed at the prominent veins causing photothermolysis and eventual closure of the capillary channel. The veins may appear reddish brown during the initial recovery period and will slowly fade over the next few weeks, with full effect of the treatment seen 4-6 weeks later. More than one session may be required to achieve complete removal of all visible reticular veins. Cryo-laser ablation is frequently combined with sclerotherapy (CLaCS) for maximal results.

Image source: (https://chic.com.mt/services/med-aesthetic-treatments/vein-treatment/)
Micro-Phlebectomies (Stab-avulsions): Micro-phlebectomy involves making small 2-3mm incisions directly over the varicose veins and removing the veins via these incisions. It is usually performed in conjunction with endovenous thermal ablation techniques (RFA/EVLT) to remove any residual tortuous veins, especially those below the knee.
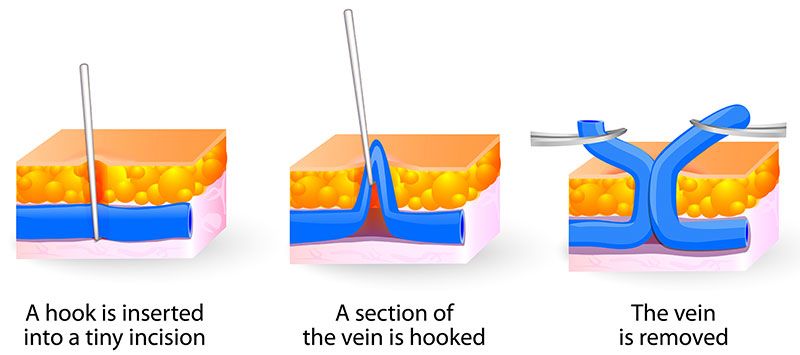
Image source: (https://www.veinspecialistofatlanta.com/vein-treatments/varicose-veins/ambulatory-micro-phlebectomy/)
What are the Risks (Complications) of Varicose Vein Surgery?
The risks are closely tied to what surgery is performed.
1. Bleeding – Some degree of bleeding is to be expected from any form of surgery, however, the amount of blood loss from varicose vein surgery is usually minimal, and blood transfusion is almost never required.
2. Infection – Bacterial infection can occur with any cut in the skin, and the risk of infection increases with the size of the wound. Most wounds for varicose vein surgery are small and thus the risk of wound infection is considered quite minimal.
3. Nerve injury – There are 2 superficial cutaneous nerves (saphenous and sural nerves) that may be injured during varicose vein surgery. If injured, they result in numbness of the skin over the lower leg. In a good majority, the numbness can recover after a few months once the nerve has regenerated. The risk of such nerve injury is highest in open vein stripping surgery and heat ablation surgery performed below the knee.
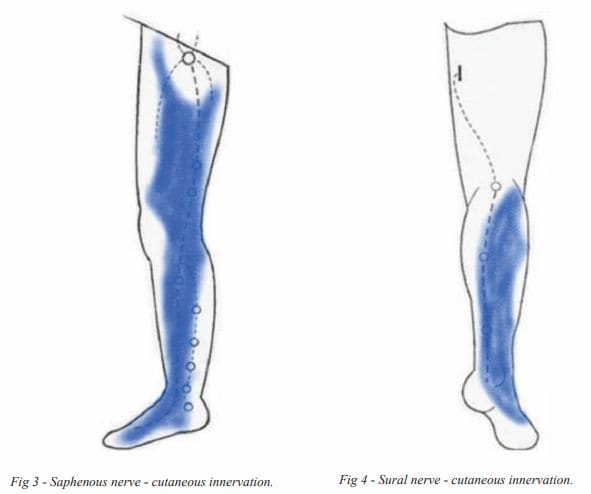
Image source: (http://www.vasculab.eu/jtavr/jtavr03/jtavr032/JTAVR000073-ArendtAL/JTAVR000073-ArendtAL.pdf)
4. Deep vein thrombosis (DVT)/Pulmonary embolism (PE) – Varicose vein surgery involves ablation of the greater saphenous vein (GSV) and/or smaller saphenous vein (SSV). These veins are connected to the deep veins in the leg at various points along its length and there is a small risk that clots can travel from the GSV/SSV into the deep veins and travel up to the lungs to cause PE. The risks are generally <1% and can be minimized by proper surgical technique.
5. Inflammation with pigmentation – Some patients may have an inflammatory reaction to the injected medication used in glue or sclerotherapy. Routine use of anti-inflammatory medications after the surgery can minimize this side effect. There may be some pigmentation seen after the inflammation has settled and steroid creams with laser therapy may be needed to lighten the pigmentation.
6. Allergy risk – There are rare reports of allergic reactions to the medication used in endovenous glue surgery. Other surgical approaches (such as endovenous heat ablation) are recommended for people with known skin allergies or those with multiple drug allergies.
What Are The Different Varicose Vein Treatments Available In Singapore?
Minimally invasive (“key-hole”) endovenous heat (RFA/EVLT) or glue ablation (VenasealTM) techniques have become the standard surgical options for varicose veins. These surgeries are frequently supplemented by either micro-phlebectomies, sclerotherapy or laser therapy to remove the smaller tortuous tributaries. Traditional open surgery is now reserved only for rare indications (such as veins with a diameter larger than 2cm). Please see “How are Varicose Veins Treated?” for details of each surgical procedure.
What Is the Recovery Time after Varicose Vein Treatment?
Varicose vein surgery is minimally invasive and is almost always performed as a day surgery procedure with the patient walking home the same day. It is recommended to engage in light activities for the first 2 weeks after the surgery and avoid complete rest in bed or long periods of immobility. Most people can return to full activity after 2 weeks from the surgery date.

Image source: (https://www.livestrong.com/article/13722249-walking-for-exercise/)
What Should I Expect After Varicose Vein Treatment?
Technical failure of varicose vein surgery is small with a reported recanalization rate of <5% after endovenous heat ablation surgery and around 10% after sclerotherapy, thus more than 90% of patients can expect to have successful treatment of their varicose veins. There is however a chance that the other veins in the leg, which were initially normal, begin to swell up and bulge out over time leading to a recurrence of varicose veins. This recurrence can be avoided by minimizing the risk factors leading to the development of varicose veins (see “What Causes Varicose Veins?” for more details).
How To Manage and Reduce the Risk of Varicose Veins
There are both modifiable and non-modifiable risk factors that contribute to the development of varicose veins (see “What Causes Varicose Veins?” for more details on the risk factors). Lifestyle changes that can be implemented to reduce the risk of varicose veins include:
- Weight reduction
- Regular graduated compression stocking wear (especially if sitting of standing for long periods)
- Avoid prolonged sitting/standing
- Avoid smoking/tobacco use
Afterword and personal comments
Varicose veins are a very common condition which if not treated early, can lead to debilitating symptoms of dry, itchy skin with unsightly pigmentation and recurrent wounds. The good news is that treatment these days is both effective and minimally invasive, allowing patients to walk home the same day of the operation.
Best results are achieved when surgery is performed for early stage (spider/reticular/varicose veins) disease. When the condition progresses to leg swelling (edema) or pigmentation (lipodermatosclerosis), treatment can only aim to minimize progression and complications, and is unable to reverse these permanent skin changes. Thus, for best results, do seek treatment as early as possible.
FAQs:
Spider veins appear on or near the surface of your skin as small blue or red lines, while varicose veins are larger veins located deeper underneath the skin that bulge out and may bleed if accidentally scratched. Please see section “What Are the Symptoms of Varicose Veins?” for a more detailed explanation of the various stages of venous disease.
Varicose veins can manifest in various ways from posing just a cosmetic issue in the early stages, to developing leg cramps and swelling, skin pigmentation and even skin ulcers. Sometimes leg swelling without the presence of any obvious varicose veins, may still be a result of venous insufficiency and an ultrasound scan will be required to detect the presence of vein disease. Please see section “What Are the Symptoms of Varicose Veins?” and “How are Varicose Veins Diagnosed (Investigations for Varicose Veins)?” for more details.
Varicose veins can cause moderate to severe discomfort depending on how advanced they are. Common symptoms include cramps and heaviness in your legs, as well as swollen ankles. They can also lead to more serious complications, such as ulcers and even blood clots, if not treated properly.
There are no home remedies that will completely eliminate the presence of varicosities, but there are a few things you can do at home to help reduce their visibility and the discomfort associated with them. These include elevating your leg when resting, wearing compression stockings, avoiding high heels, which put extra pressure on your calf muscles, and exercising regularly to improve circulation in the affected areas.
Most good insurance plans will cover treatment related to varicose veins especially if they are causing symptoms, thus making treatment a medical necessity. It is best however to check your individual plan as coverage may vary.
The surgery is successful in more than 90% of cases. Most patients will experience relief from their symptoms after just a few weeks and maintain improved circulation in the affected areas for several years following treatment. A small percentage of patients may notice varicose veins reappearing after a few years, and this is mainly due to enlargement of previously normal veins (see “What Should I Expect After Varicose Vein Treatment?” for more details). This recurrence can be avoided by minimizing the risk factors leading to the development of varicose veins (see “What Causes Varicose Veins?” for more details).
Varicose vein surgery can almost always be done without requiring an overnight hospital stay. however in certain circumstances where more complex surgery is needed, an overnight stay may be necessary. Your doctor will advise you accordingly, depending on your individual situation.
Endovenous thermal or glue ablation is usually effective at sealing off the main saphenous veins after just one session. Ablation of spider veins using sclerotherapy and/or laser therapy, may require more than one session (up to 4-6 sessions) done 4-6 weeks apart to achieve optimal results.
Varicose vein surgery improves the circulation in the leg and patients will be able to walk home the same day of the operation while maintaining light activities for the next 2 weeks. Most people can return to full activity after 2 weeks with no limitation to movement.
Lifestyle changes after successful varicose vein surgery is geared towards prevention of new varicose veins from forming. This recurrence can be avoided by minimizing the risk factors leading to the development of varicose veins (see “What Causes Varicose Veins?” for more details).
There may be slight bruising around the area where injections were administered. These however generally fade within a few hours to days. The skin incisions made during varicose vein surgery are typically 3-5mm long and once healed, are barely noticeable.
Sometimes the treated vein may appear more reddish and prominent a few days after the surgery. This discoloration usually fades after a few weeks to months, and creams or lasers may help to lighten such pigmentation should they persist.
Possible complications associated with varicose vein treatments can include infection, blood clots, or allergic reactions to certain medications used during the procedure. It is important to discuss any concerns you have with your doctor beforehand, so that they can inform you of all potential risks (see “What are the Risks (Complications) of Varicose Vein Surgery?” for more details).
The cost of varicose vein treatment in Singapore varies depending on the type of procedure chosen. You can use your Medisave and insurance to cover for your varicose vein treatment in Singapore.

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
