
OVERVIEW
A vascular malformation is an abnormal growth of the arteries, veins and/or lymphatic vessels that can occur anywhere in the body. These vessels do not develop in a normal ordered pattern but instead develop in an uncontrolled mesh-up. These malformations are usually non-cancerous but can grow and invade the tissues surrounding the malformation.
Here are some common types of vascular malformations we treat:
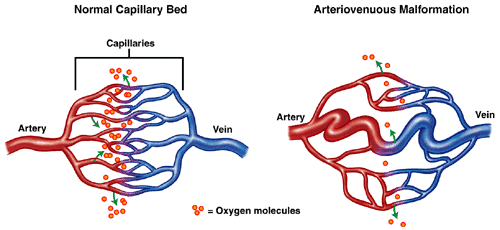
- Arteriovenous malformations (AVM): Visible abnormal growth of veins and arteries in place of capillaries. The patient may feel a pulsing sensation or thrill at the affected area.
- Venous malformations (VM): Abnormal enlargements of the wall of veins, appear as bluish or skin-coloured, soft lumps under the skin.
- Lymphovenous malformations (LVM): Lymphatic malformations are non-malignant masses consisting of fluid-filled channels caused by the abnormal lymphatic system development.
- Dural Arteriovenous Fistula: This is a rare vascular condition that occurs when abnormal connections (fistulas) are made between the arteries and veins in the brain covering (dura mater).
Hemangioma: This is a non-cancerous growth of blood vessels and commonly appears as a red birthmark on infants, which can be anywhere on the body (often on the face, scalp, back or chest).
ARTERIOVENOUS MALFORMATIONS
OVERVIEW
An arteriovenous malformation (AVM) is an abnormal tangle of blood vessels between arteries and veins that may develop shortly before or after birth affecting over 1% of the general population. AVM can be found in place of the microscopic capillaries that connect arteries and veins in our body, adversely affecting the normal blood flow.
AVMs are commonly found in the head and neck are common and may have the potential to cause severe complications, including seizures, strokes and breathing problems.
SYMPTOMS
Most AVMs do not cause any initial symptoms, and many AVMs can remain asymptomatic throughout a person’s life. However, there is a risk that the AVM will bleed, and the consequences of this can vary based on its size and severity. Symptoms can emerge at any age but usually become obvious between ages 10 to 40. Some pregnant women may experience worsened symptoms around their AVM due to increased blood pressure during pregnancy.
Symptoms include:
- Skin discolouration
- Swelling
- The skin over the AVM may be more delicate and susceptible to ulcers.
- Discomfort – pain and ache
- For brain AVMs:
- Headaches, pain in one area of the head
- Muscle weakness or numbness in a part of the body
- Seizures
- Speaking difficulty
- Confusion
CAUSES/RISK FACTORS
The causes of brain AVMs are not known, but many believe it to be congenital. Anyone can be born with an AVM, and some risk factors include:
- Family history of AVMs. It is unclear whether there is a direct correlation between family members who have had an AVM which would make it hereditary. However, it is possible to inherit other conditions that make a person more susceptible to developing an AVM.
VENOUS MALFORMATIONS
OVERVIEW
Venous malformations (VM) is the abnormal enlargement of wall of the veins, appear as bluish or skin-coloured, soft lumps under the skin. The enlarged veins result in a reduction in pressure and slower blood flow leading to blood clots formation.
SYMPTOMS
These malformations can occur anywhere in the body, and the symptoms depend on its location in the body and the type. A significant number of patients only notice the malformation and are diagnosed with it at a later age (30 – 50 years old). Even those as young as newborn infants may develop this condition, obvious symptoms usually emerge as a person ages. They include:
- Cosmetically unpleasant growths/soft lumps evident to the naked eye
- Pain and progressive discolouration of the skin around the growth
- Loss of limb function. Including muscle weakness, numbness, and in severe cases,, paralysis of a limb.
A vascular malformation inside the brain can bleed, causing a stroke or seizures (fits) due to pressure on the brain if not treated early on.
CAUSES/RISK FACTORS
Vascular malformations are mostly congenital. However, there has not been any evidence pointing to the possibility that it is inheritable. In some rare instances, vascular malformations can be caused by trauma.
LYMPHOVENOUS MALFORMATIONS
OVERVIEW
Lymphatic malformations (LVM) are rare, non-malignant masses consisting of fluid-filled spaces caused by the abnormal lymphatic system development that may appear anywhere in the body. Superficial lymphatic malformations may look like small soft bumps under the skin whereas some LVM are not visible on the surface of the body. Regardless of the LVM size, it can potentially cause functional impairment of nearby structures or organs and disfigurement of affected areas.
SYMPTOMS
Generally, symptoms of LVM arise from compression or obstruction of nearby structures and it varies depending upon the size and exact location.
Complications can occur with LVM including recurrent inflammation or bleeding into the malformation. When LVM becomes inflamed it causes swelling and redness of the skin (cellulitis). Recurrent cellulitis can result in pain and disfigurement of the affected area. Bleeding into LVM can cause severe pain, swelling and enlargement of the malformation in the affected area.
CAUSES/RISK FACTORS
Lymphatic malformation occurs when the lymph veins fail to form and develop correctly during pregnancy.
DURAL ARTERIOVENOUS FISTULA
OVERVIEW
A dural arteriovenous fistula (DAVF) is a rare vascular condition that occurs when abnormal connections (fistulas) are made between the arteries and veins in the brain covering (dura mater). When a fistula forms, blood flowing at high pressure from the arteries goes directly into the vein, which usually carries blood at a lower pressure. This can congest the brain’s venous system, ultimately leading to brain dysfunction. They are found in the brain and spine and tend to occur later in life.
SYMPTOMS
An individual with DAVF may not experience any symptoms at all. Symptoms that do appear can range from mild to more aggressive. An additional, prominent sign of DAVFs is pulsatile tinnitus. Pulsatile tinnitus occurs when a patient begins to hear the sound of blood rushing from the arteries through the fistula into the veins, characterised by a persistent whooshing to-and-fro sound near the ear. However, it is essential to note that patients suffering from pulsatile tinnitus do not always have a DAVF but may have some other condition.
Mild:
- Problems seeing
- Bulging of the eye (proptosis)
- Swelling in the eye lining
Aggressive: can often result from haemorrhages of the affected area
- Seizures
- Sudden onset of headaches
- Difficulties speaking
- Dementia
- Coordination issues
- Burning or prickling sensations around the affected area
- Nausea or vomiting
VASCULAR MALFORMATION DIAGNOSIS
Diagnosis usually is made after a clinical examination. Imaging procedures such as computerised tomography scan (CT scan or CAT scan), magnetic resonance imaging (MRI), magnetic resonance angiography (MRA) and cerebral angiogram (also known as digital subtraction angiography or DSA) may be done to determine the location and nature of the malformation as well as the degree of damage to the surrounding tissue. These tests are often repeated to check the change in the size of the AVM.
CAUSES/RISK FACTORS
There is no clear reason as to why DVAFs form. However, some patterns that have been identified include:
- Previous thrombosis vein
- Areas of the body with a history of trauma/past surgery where a fistula may develop.
- Family history of thrombosis can make a patient more susceptible to DVAFs.
- Affected age group is predominantly 50-60 years of age but may even affect children.
VASCULAR MALFORMATION DIAGNOSIS
Diagnosis usually is made after a clinical examination. Imaging procedures such as computerised tomography scan (CT scan or CAT scan), magnetic resonance imaging (MRI), magnetic resonance angiography (MRA) and cerebral angiogram (also known as digital subtraction angiography or DSA) may be done to determine the location and nature of the malformation as well as the degree of damage to the surrounding tissue. These tests are often repeated to check the change in the size of the AVM.
OUR VASCULAR MALFORMATION TREATMENTS
Surgical excision of the malformation – can recur and grow again if not completely excised and may be disfiguring. Depending on the size of the malformation, some patients may require a few sessions of such treatment.
Minimally invasive methods can instead be used to stop the growth of the malformation. Depending on the size and type of the malformation, some patients may require a few sessions of such treatment. These methods include:
- Embolisation: an interventional treatment used to block off blood flow to abnormal blood vessels, blocking off the malformed arteries. This treatment is highly effective in treating its targeted area.
Sclerotherapy: injecting the vein/lymphatic components with scarring solutions that cause the blood/lymph vessels to shrink. It is a non-surgical procedure that only requires an injection.
HEMANGIOMA
OVERVIEW
A hemangioma is a non-cancerous growth of blood vessels and commonly appears as a red birthmark on infants, which can be anywhere on the body (often on the face, scalp, back or chest). Some may also form on the internal organs of the body. A significant number of hemangiomas disappear by the time a child turns six years old, resolving themselves with no further treatment required. However, in some children, hemangiomas may persist.
SYMPTOMS
The majority of hemangiomas do not cause any noticeable signs or symptoms, aside from the appearance of the red birthmarks that are smooth and raised in appearance. Once it disappears, the skin may be slightly discoloured in the area the hemangioma previously occupied, and a small lump in the skin may persist.
However, in some cases, hemangiomas may bleed and develop into a sore, resulting in pain and the potential for infection. Hemangiomas on the organs can also cause some complications, including pain where it is located, although this is very rare.
CAUSES/ RISK FACTORS
The physical appearance of a hemangioma is caused by the clumping together of blood vessels. However, an exact reason for why this occurs has not been identified.
It has been noted that infantile hemangiomas are more common in the following:
- infants with low birth weight
- premature infants
- Multiple births (e.g. twins/triplets)
PROCEDURES/ TREATMENTS
Hemangiomas may be resolved through the use of medication, including propranolol and beta-blockers. However, interventional therapies provide an alternative treatment method for those that do not respond to medication or for patients who would prefer a non-pharmacological route.
- Sclerotherapy – It is a minimally invasive procedure that involves the injection of a chemical solution into a blood vessel. This agent causes inflammation in the blood vessel walls resulting in the blood vessel occlusion.
- Laser Therapy – Lasers may be used to remove blood vessels that remain on the surface and minimise any abnormalities left by the hemangioma, such as unevenness of the skin.
References:
