
OVERVIEW
The aorta is the largest artery in the body. It is the main blood vessel that carries blood from the heart to the rest of the body. It extends from the heart into the chest, down to the abdomen and into the pelvis. From there, it then goes down to form the main blood supply to the legs. During its course, the aorta gives off vital branches that form the key arterial blood supply to vital organs such as the liver, stomach, intestines and kidneys.
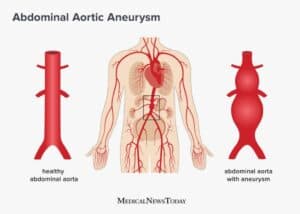
An Aortic Aneurysm (AA) develops when the wall of the aorta weakens and begins to bulge outwards like a balloon.
There are several regions where an aortic aneurysm may develop:
- In the chest: Thoracic Aortic Aneurysm (TAA)
- In the abdomen: Abdominal Aortic Aneurysm (AAA)
- Between the chest and abdomen: Thoracoabdominal Aortic Aneurysm (TAAA)
In its early stages, when an AA is small in size, it does not pose an immediate health risk. However, if the AA continues to grow, the walls of the aorta or its lower branches can become thin and lose their ability to stretch. The weakened sections of the wall may become unable to support the force and pressure of blood flow. Such an aneurysm could burst, causing severe internal bleeding and death.
SYMPTOMS
- Pain – persistent and severe pain in the chest, abdomen, and back or the lower limbs
- Persistent fever
- Pulsating or throbbing mass in the abdomen
- Gangrene patches in the toes
- Recurrent vomiting after eating
CAUSES/RISK FACTORS
Patients are advised to undergo screening if they belong to the following risk factor groups:
- Chronic smokers
- Older than 65 yrs, predominantly males
- Long-term hypertension and/or heart disease
- Those with congenital soft tissue diseases such as Marfan’ syndrome, Ehlers-Danlos Syndrome, Loeys-Dietz Syndrome
- Strong family history of aortic aneurysms and dissections
DIAGNOSIS
Diagnosis is based on clinical examination where an aneurysm can be felt as a throbbing mass in the abdomen. An ultrasound scan or CT scan is recommended for confirmation of an aneurysm
OUR TREATMENTS
There are two types of treatment for AA:
- Open Surgical Repair – This is the conventional method of aneurysm repair that involves making long incisions on the chest wall.
- Open surgical repair is a robust method but has significant morbidity and mortality risks due to its invasive nature that is recommended only for younger patients with low surgical risk. Post-surgery recovery usually requires ICU care for up to 1 week. Patients generally take about one month to 6 weeks to full recovery.
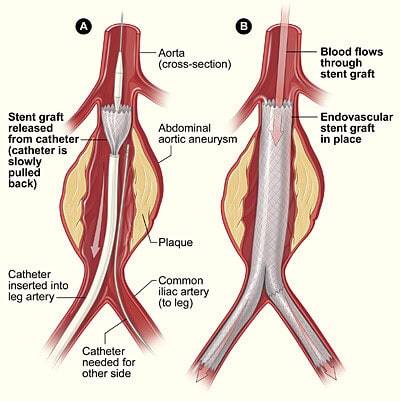
- Minimally Invasive Repair – This method uses covered stent-grafts, also known as EndoVascular Aortic Repair (EVAR). It involves the insertion of special stents (small tubes that hold the vessel open) through the leg femoral arteries via small (1cm) incisions in the groin into site of aneurysm, relining the stent and excluding it from the arterial blood pressure circulation under X-ray guidance (fluoroscopy)
- EVAR can be done for older patients or patients with many comorbidities who have higher surgical risks. Also, due to its minimally invasive nature, EVAR can be done under local anaesthetic and mild sedation. Patients who undergo EVAR usually do not require ICU stay and are patients are up and about in 8 hours and are discharged 48 hours post-surgery. In selected cases, young and fit patients can even be discharged on the same day.
FOLLOW-UP CARE
After the AA has been treated, all patients should have regular follow-ups for the rest of their life. This is because the disease can continue to develop in other parts of the aorta that were previously aneurysm-free. It is not uncommon for a patient with an abdominal aneurysm to then develop a thoracic aneurysm and vice versa. This is especially so if the patient still has persistent risk factors such as smoking and hypertension.
Follow-up post aneurysm repair requires repeat ultrasound scans and CT scans to be done at regular intervals (6 monthly at first and then annually). This is particularly important for patients who have undergone the EVAR procedure and the scans are done to detect leaks around the covered stent graft.
AORTIC DISSECTION
OVERVIEW
An aortic dissection occurs when there is a tear in the wall of the aorta, resulting in blood flowing in between the muscle layers of the aorta. As a result, the aorta is divided into two openings instead of one. An aortic dissection can disrupt flow into the artery branches and organs supplied by the aorta, including the intestines, kidneys and legs, ultimately causing organ failure.
SYMPTOMS
- Severe chest pain associated with elevated blood pressure
- Local abdominal pain and tenderness
CAUSES/RISK FACTORS
At-risk groups include:
- Those suffering from uncontrolled hypertension
- Those with congenital soft tissue diseases such as Marfan’ syndrome, Ehlers-Danlos Syndrome, Loeys-Dietz Syndrome
- Those who may have sustained trauma to the aorta e.g a motor vehicle accident
DIAGNOSIS
A contrast CT scan of the chest and abdomen is the best way to diagnose an aortic dissection. It will also reveal where the initial tear in the aortic wall is, the extent of the dissection (which parts of the aorta is involved) and the affected organs/blood supply. This will give the doctors an idea of the best way to treat the dissection
OUR TREATMENTS
The immediate priority will be to control the elevated blood pressure so that the dissection does not worsen.
The next step is either open surgery to repair the tear of the aortic wall or minimally invasive EVAR – the insertion of a stent-graft through the groin arteries.
Kandola, A. (2020, May 27). Abdominal aortic aneurysm: Screening, treatment, and symptoms. Retrieved January 25, 2022, from https://www.medicalnewstoday.com/articles/abdominal-aortic-aneurysm
References:
