Carotid arteries, vital vessels in your neck, supply blood to your brain and head. Carotid artery disease occurs when these arteries narrow due to plaque buildup, mainly fat, cholesterol, and calcium. This condition can lead to blockages, potentially causing strokes. While symptoms might not manifest until severe narrowing occurs, signs like a distinctive sound on auscultation of the neck or a transient ischemic attack (TIA) can indicate trouble.
(https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/symptoms-causes/syc-20360519)
Introduction to Carotid Artery Disease
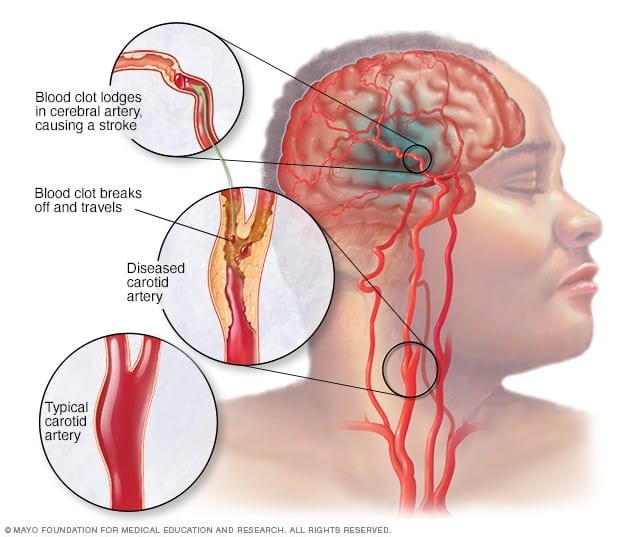
Carotid Artery Disease (CAD) arises when the main neck arteries that supply the brain become narrowed and obstructed by fatty plaque deposits, a condition known as atherosclerosis. This disease significantly raises the risk of ischemic strokes, which occur when the brain’s blood supply is compromised. CAD is responsible for some cases of strokes, and it can ultimately lead to severe consequences such as brain damage, muscle weakness, and even death. The disease’s detrimental effects stem from various mechanisms, including reduced blood flow due to narrowed arteries, the potential rupture of plaques leading to blockages in smaller brain arteries, and the formation of blood clots that obstruct blood flow. Strokes, caused by oxygen deprivation to the brain resulting in rapid cell death, rank as a major cause of death and disability. Carotid artery disease often progresses gradually and may first manifest as a stroke or a transient ischemic attack (TIA), a temporary disruption of brain blood flow. Carotid artery disease treatment typically encompasses lifestyle adjustments, medication, and in some cases, surgical intervention.
Symptoms of Carotid Artery Disease
Patients diagnosed with CAD often remain asymptomatic until a stroke or transient ischemic stroke, often referred to as a “ministroke,” occurs. Stroke symptoms include difficulties in speech and comprehension, potential confusion or slurred speech, paralysis or numbness on one side of the body (such as the face, arms, or legs), impaired arm-raising ability, facial drooping, hand tremors, sudden dizziness, loss of balance and coordination, sudden vision problems or light sensitivity in one or both eyes, intense and sudden headaches, nausea, vomiting, challenges in swallowing, and loss of consciousness.
Causes and Risk Factors of Carotid Artery Disease
Carotid artery disease risk factors encompass various causes:
- Age: Atherosclerosis, the foundation of CAD, may initiate in youth and gradually evolve into stroke and CAD with advancing age.
- Family History: A positive family history of stroke or atherosclerosis heightens risk.
- Previous Stroke: A history of stroke elevates susceptibility.
- High Blood Pressure: Hypertension increases the likelihood of CAD.
- High Cholesterol: Elevated cholesterol levels contribute to plaque formation.
- Obesity and Inactivity: Being overweight or leading a sedentary lifestyle amplifies the risk.
- Diabetes: Diabetic conditions enhance vulnerability.
- Smoking: Tobacco use is a significant risk factor.
Carotid artery disease emerges from the accumulation of plaques, composed of cholesterol, fat, and blood cells, within the arteries responsible for brain blood supply. This process, termed atherosclerosis, leads to the narrowing of carotid arteries. Consequently, the obstruction impedes the delivery of oxygen and nutrients to the brain.
Diagnosis of Carotid Artery Disease
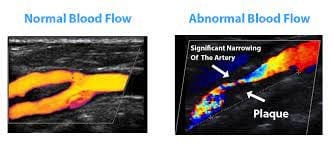
In the process of diagnosing carotid artery disease (CAD), specific scans and screenings are performed, especially for individuals considered high-risk. These diagnostic approaches encompass a range of imaging tests, including ultrasound, head CT scan, MRI scan, and MRA (Magnetic Resonance Angiography). Additionally, a cerebral angiogram, also known as Digital Subtraction Angiography (DSA), may be utilized. This procedure, which is minimally invasive, entails the insertion of dye into the carotid artery via a catheter, allowing for the capture of an X-ray image to assess the condition of the arteries.
(https://ultrasound.ie/the-carotid-doppler-ultrasound/)
Treatment Options for Carotid Artery Disease
In the realm of atherosclerosis treatment, a multifaceted approach is available to patients, encompassing both lifestyle adjustments and medical interventions to effectively manage risk factors and potentially deter or delay the onset of carotid artery disease (CAD). Should lifestyle changes prove inadequate, medical professionals might advocate for medications or minimally invasive surgical procedures.
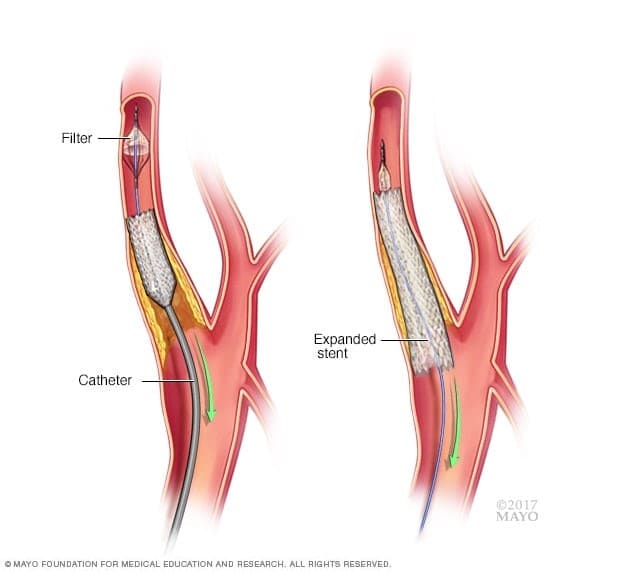
One such intervention is angioplasty and stenting, regarded as a minimally invasive and highly efficacious treatment option. This procedure involves the dilation of arteries to reinstate optimal blood flow to the brain. A catheter is carefully inserted into the affected artery, through which a balloon is maneuvered and then inflated to expand the artery’s diameter. Following this, a stent – a supportive device – is positioned within the artery to fortify its walls, mitigating the risk of future narrowing.
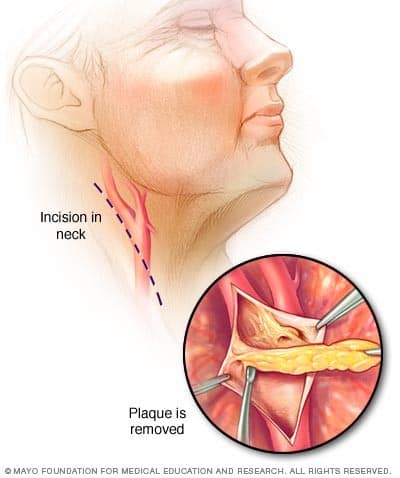
Alternatively, open surgery in the form of endarterectomy remains a traditional means of addressing CAD. This surgical technique necessitates an incision in the neck, facilitating access to the compromised artery. The vascular surgeon then removes the accumulated plaque or obstruction from the artery’s inner lining, thus reinstating unimpeded blood flow. Ultimately, the treatment approach for atherosclerosis and CAD is tailored to the individual patient’s condition, risk factors, and overall health, with the goal of mitigating the impact of the disease and optimizing the patient’s well-being.
(https://www.mayoclinic.org/tests-procedures/carotid-endarterectomy/about/pac-20393379)
Lifestyle Changes for Carotid Artery Disease
The main objective in managing carotid artery disease is to prevent the occurrence of a stroke.
- Kick the smoking habit. Within a few years of quitting, a former smoker’s stroke risk aligns with that of a nonsmoker.
- Sustain a balanced weight. Shedding excess pounds mitigates the exacerbation of other risk factors, including high blood pressure, cardiovascular ailments, diabetes, and sleep apnea.
- Embrace a nourishing diet. Prioritize a consumption pattern rich in fruits, vegetables, whole grains, fish, nuts, and legumes. Restrict the intake of cholesterol and fats, particularly saturated and trans fats.
- Moderation in salt intake. Excessive salt consumption can elevate blood pressure in certain individuals.
- Regular physical activity. Engaging in routine exercise contributes to blood pressure reduction and bolsters the overall vitality of blood vessels and the heart. It also aids in weight management, diabetes control, and stress reduction.
- Exercise prudence or abstinence regarding alcohol. If alcohol is part of your lifestyle, do so judiciously.
- Manage health conditions. Effectively handling illnesses like diabetes and high blood pressure offers a safeguard for arteries, shielding them from potential harm.
Risks Associated with Carotid Artery Disease Surgery
Carotid endarterectomy comes with a set of potential risks that warrant careful consideration. These include the likelihood of experiencing a stroke or transient ischemic attack (TIA), both of which constitute potential neurological complications. Additionally, the procedure carries a risk of heart attack, posing a potential threat to cardiovascular well-being. One possible outcome is the pooling of blood around the incision site, leading to post-operative swelling and discomfort. Moreover, there is a chance of nerve-related issues affecting sensory functions such as eyesight, smell, taste, or hearing. Intracerebral haemorrhage, characterized by bleeding into the brain, is another potential but rare complication. Seizures, though uncommon, can also occur because of the procedure.
Lastly, there exists a potential for airway obstruction, stemming from post-operative swelling or bleeding in the neck. To make an informed decision, it is crucial to engage in a comprehensive discussion of these potential risks with your healthcare provider prior to undergoing the carotid endarterectomy.
Benefits of Angioplasty and Stenting
The advantages of angioplasty and stenting are in their minimally invasive nature and their efficacy in restoring blood flow to the brain. This treatment involves inserting a catheter into the artery and using a balloon to widen the arteries by compressing plaque deposits. A stent is subsequently positioned within the artery to provide structural support, preventing future narrowing. This approach not only effectively addresses blockages but also maintains improved blood flow, offering a comprehensive solution for patients with reduced blood flow to the head.
(https://www.mayoclinic.org/tests-procedures/carotid-angioplasty-and-stenting/about/pac-20385111)
Final Words
Carotid Artery Disease (CAD) occurs when neck arteries supplying the brain narrow due to fatty plaques, increasing stroke risk. This condition can lead to severe consequences such as brain damage and death. CAD’s effects include reduced blood flow, plaque rupture, and blood clot formation, causing strokes. Diagnosis involves imaging tests, and treatment options range from lifestyle changes and medications to minimally invasive procedures like angioplasty and stenting, or traditional open surgery. Consulting a vascular surgeon is vital for informed decisions.
FAQs:
Carotid Artery Disease (CAD) occurs when neck arteries supplying the brain narrow due to fatty plaques, heightening stroke risk. It can lead to severe consequences like brain damage and death, stemming from reduced blood flow, plaque rupture, and clot formation. Strokes, caused by oxygen deprivation and rapid cell death, are a significant cause of disability and death. CAD progression is gradual and may manifest as strokes or temporary disruptions of blood flow. Treatment involves lifestyle changes, medication, and possibly surgery.
CAD patients are often asymptomatic until a stroke or “ministroke” happens. Stroke signs comprise speech issues, confusion, numbness, paralysis on one side, facial drooping, dizziness, vision problems, severe headaches, nausea, and loss of consciousness.
Carotid artery disease risk factors include age, family history, previous stroke, high blood pressure, high cholesterol, obesity, inactivity, diabetes, and smoking. Atherosclerosis, characterized by plaque buildup of cholesterol, fat, and blood cells, narrows carotid arteries, reducing oxygen and nutrient supply to the brain.
Diagnosing carotid artery disease (CAD) involves specialized scans and screenings, particularly for high-risk individuals. These include ultrasound, head CT scan, MRI scan, and MRA. Another option is a minimally invasive cerebral angiogram, where dye is injected into the carotid artery via a catheter to capture X-ray images for assessing artery condition.
A comprehensive approach to treating atherosclerosis involves lifestyle changes and medical interventions to manage risk factors and potentially prevent carotid artery disease (CAD). Medical options include angioplasty and stenting, which restore blood flow via minimally invasive procedures, or endarterectomy, a surgical technique that removes arterial plaque. Treatment is personalized based on individual health and aims to reduce disease impact and enhance well-being.
Angioplasty and stenting, a minimally invasive and effective treatment, involve widening arteries to restore optimal blood flow to the brain. A catheter is inserted into the affected artery, a balloon is inflated to expand the artery, and a stent is placed to support the artery’s walls and prevent future narrowing.
This procedure involves making an incision in the neck to access the affected artery, allowing the surgeon to remove plaque and obstructions from the artery’s inner lining, restoring normal blood flow.
To mitigate the risk of carotid artery disease, it’s crucial to quit smoking, maintain a balanced weight, adopt a nourishing diet, limit salt intake, engage in regular physical activity, practice moderation with alcohol, and effectively manage underlying health conditions.
Carotid endarterectomy poses potential risks including stroke, heart attack, bleeding, nerve-related issues, intracerebral haemorrhage, and seizures. Recurrent blockages, infection, blood pressure impact, irregular heartbeat, and airway obstruction are also concerns, underscoring the importance of discussing these risks with your healthcare provider before undergoing the procedure.
Angioplasty and stenting offer minimally invasive and effective solutions for restoring blood flow to the brain by widening arteries and placing a supportive stent. Compared to open surgery, they offer benefits such as smaller incisions, quicker recovery, shorter hospital stays, and improved cardiovascular health.
References:
[1] https://www.webmd.com/heart-disease/carotid-artery-disease-causes-symptoms-tests-and-treatment
[2] https://my.clevelandclinic.org/health/diseases/16845-carotid-artery-disease-carotid-artery-stenosis
[3] https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/symptoms-causes/syc-20360519

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
