- Is there a pelvic congestion syndrome specialist near me?
Vascular and Interventional Centre is here to address your vascular needs through holistic medicine and customised treatments. Contact +65 6694 6270 to book an appointment with our team of well-trained vascular specialists.
A woman’s reproductive system is a highly complex and intricate system that requires a lot of care and attention. It is an integral part of a woman’s overall health and wellness, and it should be regarded as such.
Pelvic pain is something that many women experience in Singapore, and it is highly likely that your female relatives, friends, and colleagues have gone through this same problem. A congested pelvic area can be linked to numerous factors, ranging from harmless menstruation-related symptoms to a sign of a life-threatening sickness.
Pelvic pain may be caused by problems with nonreproductive organs (like the bladder or bowel) or reproductive organs (like the ovaries or uterus). Finding the exact root cause of pelvic pain requires a comprehensive assessment and advice from a specialist who is aware of all the possible conditions, and who can provide a holistic assessment to reach the correct diagnosis.
Many women attribute frequent pelvic pain to their normal menstrual cycle or other benign intestinal or urinary issues. However, pelvic pain occasionally may be due to more serious medical conditions such as endometriosis, pelvic congestion syndrome or even pelvic organ malignancies. Thus, it is highly recommended to seek advice from a specialist if you experience recurrent pelvic pain, especially if the discomfort frequently requires painkillers to control, or leads to time off work and affects your regular activities.
(https://www.myaimhealth.com/pelvic-2-3/)
What is Pelvic Congestion Syndrome?
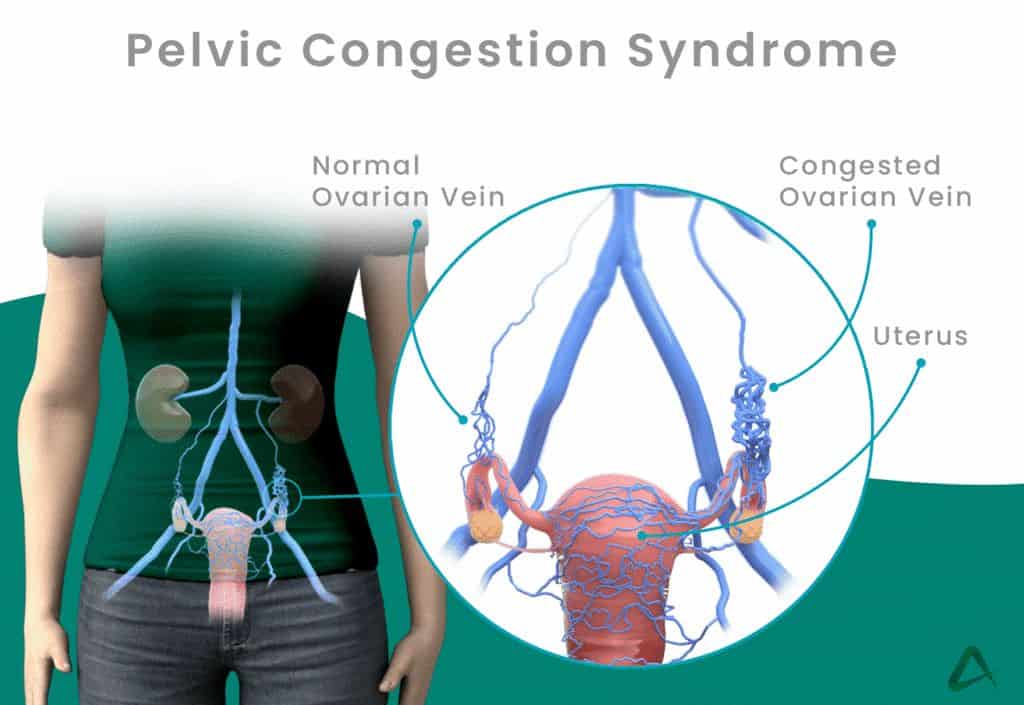
Pelvic congestion syndrome (PCS), also called pelvic venous insufficiency, is a chronic condition that affects females mainly between the ages of 20 to 45. Those who have experienced childbirth more than once are also at higher risk. The exact cause of pelvic congestion syndrome is not well understood, but the increased pelvic blood flow during pregnancy which leads to dilatation of the veins, which in turn leads to weakening of the valves, is believed to be a contributing cause. The pain and discomfort experienced by pelvic congestion syndrome is due to the pooling of blood in the pelvic veins due to the malfunctioning valves, thus causing stretching of the veins and the accompanying pain associated with this phenomenon.
There is a paucity of awareness of pelvic congestion syndrome, and it is actually more common than most people realise. It is estimated that up to 40% of women who have gynaecological visits complain of chronic pelvic pain, and approximately 30% of these visits are closely connected to pelvic congestion syndrome.
What causes Pelvic Congestion Syndrome?
Even after decades of research, there is found to be no singular cause to Pelvic Congestion Syndrome. It is attributed to several bodily functions, all surrounding dysfunctional pelvic veins and ovarian veins. In your veins, there are valves that let blood flow to a single direction. These valves close to prevent blood from flowing backwards, which can negatively impact the supposed blood flow by interrupting important bodily functions. When this happens, you may suffer from varicose veins or varicosities, which occurs when veins become twisted, dilated, and overflow with blood.
Varicose veins around the ovaries can result in prolonged pain from interrupted blood flow in malfunctioning and congested veins. When the valves weaken, they are not able to prevent blood from flowing backward. There becomes a reflux of blood, which is often accompanied by pain and discomfort around the pelvic area. Since the veins cannot handle the sudden onset of blood, the veins tend to stretch and twist.
It is a common misconception that varicose veins are only found in the leg area. In reality, varicose veins can also develop in your pelvic area. Some researchers believe that the emergence of varicose veins in the pelvis is rooted in pregnancy. When a person gets pregnant, they undergo major body changes. The body tries to compensate for the extra processes by producing extra blood which makes the heart pump faster than the normal rate. As the body’s needs increase, it exerts more effort to produce nutrients and keep up with natural processes of growing a foetus.
With all the hormonal imbalances, weight gain, body aches, and other physical changes, your veins may be affected by circulation issues. This onset of stress may prevent veins from properly functioning. Since chronic pelvic pain is a symptom of both pregnancy and Pelvic Congestion Syndrome, it becomes increasingly important for women to seek professional advice from doctors and specialists.
In addition to this, women in the menopausal stage rarely develop Pelvic Congestion Syndrome. This may be linked to hormonal changes, with the female body producing increased amounts of oestrogen during pregnancy. Oestrogen is linked to the dilation or widening of the veins, which may lead to circulation issues. When a woman is experiencing menopause, she no longer ovulates and there is a decreased level of oestrogen production. Even so, there is an extremely rare chance that menopausal women can still acquire Pelvic Congestion Syndrome.
What are the risk factors associated with Pelvic Congestion Syndrome?
There are several risk factors that increase the likelihood of developing Pelvic Congestion Syndrome. Though it is not a lethal condition, it still warrants specific treatments to avoid functional disability and recurring pain. If you identify with any of these risk factors, it would be wise to take extra steps to stay healthy.
- Age – It typically affects 20- to 45-year-old women. Chronic pelvic pain is also a common occurrence of women in this age group. It causes discomfort which can affect daily activities such as work and school, having a negative impact on efficiency.
- Life stage – It is prevalent in women who are in their childbearing years. There are numerous reproductive health concerns for women in their peak reproductive years, including endometriosis and uterine fibroids. All of these are characterised by pelvic pain, which makes diagnosis difficult.
- Frequency of pregnancy – It is more common for women who have given birth two or more times to develop Pelvic Congestion Syndrome. The repeated stress of multiple childbirths affects the veins around the pelvic area, causing valves to weaken and malfunction.
- Family history – Some inherited genes make women more likely to develop Pelvic Congestion Syndrome. This highlights the importance of understanding one’s family health history. This condition is not preventable, but there are treatments to help with pain management.
What are the various signs and symptoms of Pelvic Congestion Syndrome?
The signs and symptoms of this condition manifests differently for everyone. Keep in mind, one should visit a healthcare provider even before symptoms become too severe. While some symptoms are persistent and come regularly, others may disappear for a while and then come back at a later time. It is important to remember that Pelvic Congestion Syndrome is highly complex, since its symptoms differ from one patient to another. If you are in doubt, it is best to contact a healthcare provider to ease your mind.
It is important to keep track of the first occurrence of these symptoms. Your medical provider will inquire about your medical history and symptoms to properly identify or rule out Pelvic Congestion Syndrome. These symptoms depend on various factors such as physical condition, lifestyle changes, and many more.
1. Pelvic pain – The pain may oftentimes feel dull or heavy, while some can experience sharp and severe pain. It may come in sporadic or continuous patterns.
a. Area of the body – Pelvic pain can be felt in the lower abdomen, below the belly button. Some women also experience back pain particularly in the lumbar region. It is characterised by a feeling of dull or intense pressure.

(https://www.ivyrehab.com/news/what-causes-pelvic-pain/)
b.Pregnancy – The pain may appear during or after pregnancy. As mentioned earlier, it may potentially worsen after multiple pregnancies because the veins may be damaged permanently. Veins widen and enlarge during pregnancy to accommodate increased blood flow.
c.Time of the day – The pain associated with Pelvic Congestion Syndrome can be felt at any time, but it can get worse at the end of the day. The pain may be exacerbated by menstrual pain which comes before and during the period itself.
d.Menstruation cycle – The pain may feel more excruciating during the premenstrual stage and during the actual menstruation stage. It may also cause irregular periods, in which the length and duration of the cycle keep changing. This may lead to abnormal period bleeding, a heavier flow than usual, and painful cramps felt in the lower abdomen.
e.Sexual intercourse – Dyspareunia is recurrent genital pain that may appear during and after intercourse. The feeling is similar to menstrual cramps, with a dull continuous ache.
f.Daily activities – The pain may worsen when sitting or standing for prolonged periods of time. For some, pelvic pain gets worse after strenuous exercise. It may lessen or completely disappear when lying down.
2.Varicose veins – Pelvic veins are closely connected to veins in the limbs. As a result, varicose veins can form on the legs, vulva, thighs, and buttocks. A growing foetus and anatomical changes result in stressed and swollen veins particularly in these areas.

(https://crowsnestcosmeticandvein.com.au/are-varicose-veins-dangerous/)
3.Digestive problems – This condition can cause bloating or swelling of the stomach, diarrhoea, and constipation. The damaged veins disrupt the function of the pelvis, which negatively affects the digestive organs such as the bowel.
4.Stress incontinence – There is an involuntary loss of urine when there is abdominal pressure from sneezing, laughing, or performing other actions. The affected veins disrupt the bladder, which may also cause painful urination accompanied by a burning feeling.
5.Haemorrhoids – Pelvic vein issues may cause haemorrhoids, which are swollen veins in the anus and rectum. This may be linked to constipation or bowel movement problems which cause itching and irritation.
6.Leg fullness and swelling – Chronic pelvic pain may spread to other parts of the body. It can affect the lower back, buttocks, thighs, and legs. One may feel pain coming from the pelvis that slowly radiates down to the leg area.
What are conditions share similar symptoms with Pelvic Congestion Syndrome?
Chronic pelvic pain and other previously mentioned symptoms are linked to several other conditions. Since chronic pelvic pain is a common occurrence, it can be classified as a symptom in digestive, circulatory, urinary, and nervous system conditions.
- Menstrual Cramps – Cramps occur when the muscles of the uterus contract. Some women experience mild to extreme pain in the lower abdomen area when the uterus sheds its lining. As the hormones change, the menstrual cycle also affects bowel movements.
- Uterine Fibroids – Fibroids are common benign growths in the uterus. It is characterised by pelvic pain, backaches, irregular period flow and patterns, and painful sexual intercourse among other symptoms. Fibroids commonly cause pain when doing exercises and even daily activities.
- Reproductive Tract Cancer – Gynaecologic cancers often manifest through chronic pelvic pain, painful urination, bloating, constipation, painful sexual intercourse, and fatigue. Pelvic pressure is an early indicator of ovarian cancer, where there is a lack of blood supply to the ovary.
- Endometriosis – Endometriosis, which is the growth of tissue outside the uterus, is characterised by severe pain during menstruation, sexual intercourse, urination, bowel movements, and nausea. It is associated with infertility and several mental health issues such as anxiety and depression.
- Urinary Tract Infection (UTI) – This is a bacterial infection of the urinary system, which can include the bladder, kidney, and urethra. Women may experience painful urination, pelvic or abdominal pain, and fevers. An early symptom of UTI is a burning feeling when urinating and a feeling of fullness in the bladder.
- Polycystic Ovary Syndrome (PCOS) – This hormonal condition causes infertility, mood changes, pelvic pain, acne, irregular menstruation, digestive issues, and excess hair growth. The discomfort originates from cysts in the ovary which can range from a dull ache to a sharp pain.
- Pelvic Inflammatory Disease (PID) – The inflammation of the female genital tract is distinguished by abdominal pain, fevers, bleeding between periods, pelvic pain during sexual intercourse, and heavy vaginal discharge. This ailment may cause damage to the uterus, cervix, and fallopian tubes.
- Ectopic pregnancy – This condition happens when a fertilised egg attaches itself to the fallopian tube, cervix, and other locations outside the uterus. Severe pain in the abdomen and pelvis, bleeding in between periods, fatigue, and rectal pressure are signs of an ectopic pregnancy.
- Ovarian cyst – Ovarian cysts are common liquid-filled sacs that form during the menstrual cycle. These are usually harmless, but some become cancerous over time. Cysts may manifest through pelvic pain, frequent urination, irregular periods, and painful sexual intercourse.
- Hernia – A hernia happens when the abdominal muscles weaken and cause tearing. Its symptoms include strained bowel movement, bloating, and a physical bulge in the pelvic area. The pain or feeling of discomfort may worsen when performing physical activities.
What is Pelvic Congestion Syndrome’s impact on fertility?
There is a chance that women will experience fertility problems if they are diagnosed with Pelvic Congestion Syndrome. The affected veins may cause the uterus, ovaries, and fallopian tubes to malfunction. This is associated with chronic pelvic pain, which depends on the underlying cause and risk factors of the individual. Pelvic Congestion Syndrome can also cause difficulties in sexual intercourse, making it much more strenuous to conceive.
Women who have gone through multiple pregnancies are more likely to have fertility problems after being diagnosed with Pelvic Congestion Syndrome. As pelvic veins become damaged through constant pressure, reproductive organs may cease to function. Nonetheless, being diagnosed with Pelvic Congestion Syndrome does not automatically make you infertile.
Some treatments for Pelvic Congestion Syndrome directly affect fertility. People who undergo a hysterectomy, which is the removal of the uterus, do not experience menstrual periods after the operation. As a result, they cannot get pregnant anymore. Even so, it is ultimately up to your doctor to decide on a proper treatment. There are other procedures like Pelvic and Ovarian Vein Embolisation Surgery, which is a minimally invasive procedure that blocks off faulty veins and decongests the pelvis.
How can Pelvic Congestion Syndrome be diagnosed?
A vascular doctor is a specialist in the treatment of ailments of the vascular system which includes blood vessels and veins. Once you secure a medical appointment with a vascular specialist, they will ask questions about your symptoms, medical history, existing medications, lifestyle, and other factors. They may conduct the following procedures for diagnosis:
1.CT scan – This procedure uses computers and X-ray machines to produce images of the inside of the body. A CT scan shows a detailed visual of the veins in the pelvic region.
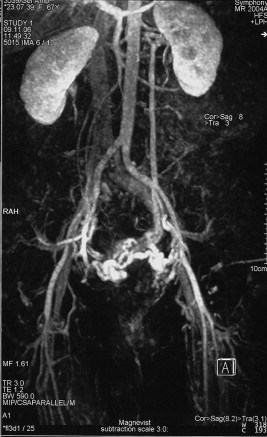
(https://www.sciencedirect.com/science/article/pii/S1078588408003626)
2.Pelvic venogram – This method involves injecting a contrast agent or dye into the pelvic organ veins using a catheter. A pelvic venogram makes the veins more visible.
3.Ultrasound – Similar to the CT scan, this procedure involves a machine to generate live images of the body. It can provide a visualisation of the pelvic area and its related structures.
4.Laparoscopy – This is a minimally invasive process where a vascular surgeon makes tiny cuts through the abdomen. A laparoscopy enables medical professionals to view and assess reproductive organs.
5.Blood and urine tests – These tests may be required to rule out other conditions and pinpoint the exact cause of pelvic pain and other symptoms. A blood test can detect sexually transmitted diseases and pregnancy, while a urine test can detect urinary tract infections and diabetes.
What are the treatment options for Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome is hard to diagnose, but it is not difficult to treat. There are many effective medications and procedures available to alleviate your symptoms.
Non-surgical management
- Anti-inflammatory drugs and hormonal medications – This method can relieve pain by improving blood flow and decongesting varicose veins. Since oestrogen is linked to the widening or dilation of veins, medications which suppress oestrogen production can help alleviate symptoms.
Surgical management
- Salpingo-oophorectomy – A medical professional may recommend performing a bilateral salpingo-oophorectomy, which is the process or removing pelvic organs such as the ovaries and fallopian tubes. Even so, this surgery is very rare for those who are experiencing Pelvic Congestion Syndrome.
- Hysterectomy – Similar to the aforementioned surgery, a hysterectomy involves removing the entire womb or uterus. Women who have underwent a hysterectomy cannot conceive or get pregnant after this operation.
What is Pelvic and Ovarian Vein Embolisation Surgery?
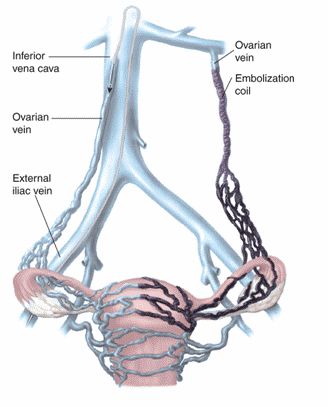
This is one of the most common procedures to treat Pelvic Congestion Syndrome. It is a minimally invasive method, which means that it involves tiny incisions which reduce possible surgery-related injuries. With minimally invasive procedures, patients enjoy shorter recovery times compared to those who undergo open surgery. Pelvic and Ovarian Vein Embolisation Surgery follows this procedure:
- A thin tube called a catheter is inserted into the affected veins in the pelvis and ovaries via a small puncture wound in the groin or arm.
- The vascular surgeon performing the procedure is guided by fluoroscopy, which is an x-ray imaging technique which produces real-time imaging of the vessels in the body.
- Through the catheter, tiny titanium coils are sent into the damaged veins. These coils will cause the damaged veins to close permanently.
- After the veins close and the blood flow is redistributed, the body’s organs are relieved from the chronic pain brought on by a congested pelvis.
(https://lavascular.com/pelvic-congestion-syndrome/)
What should I expect after I get treated for Pelvic Congestion Syndrome?
75% of patients who undergo Pelvic and Ovarian Vein Embolisation Surgery experience relief from the pains and discomfort associated with the condition. You can expect the following after the surgery:
- Same-day discharge – Those who undergo minimally invasive procedures like vein embolisation get to go home right after being cleared from the operation.
- Minimal pain and discomfort – Since the operation generally involves tiny incisions, the patient is expected to have a quick recovery.
- Quick return to daily activities – Minimally invasive surgery is associated with faster healing and shorter duration of post-surgery pain.
- Follow-ups or check-ups with the healthcare provider – Aftercare is an important aspect of patient recovery. A follow-up test may be conducted by a doctor to ensure full recuperation and healing.
As with other patients who go through a medical procedure, a balanced diet, regular exercise, sufficient rest, and support from loved ones are all necessary for a smooth recovery. There are several tips to maintain a healthy lifestyle and achieve a quick recovery:
- Eat healthy meals – Choose your food carefully and limit your intake of unhealthy food.
- Watch your weight – Integrate fruits and vegetables into your diet and set health-related goals.
- Stay hydrated – Drink more water to regulate body temperature and promote organ function.
- Exercise regularly – Move your body and stay active by walking, jogging, or doing yoga.
- Get good sleep – Set up a nighttime routine to wind down after a tiring day.
- Manage stress and emotions – Enjoy your hobbies and explore effective stress management techniques.
- Take vitamins and supplements – Integrate vitamins into your routine and get the most out of your meals.
- Take a well-deserved time out – Enjoy a break from school or work and focus on self-healing.
- Nurture social relationships – Communicate with loved ones and forge healthy relationships.
- Avoid smoking and drinking alcohol – Avoid temptation and flush out unhealthy habits.
Final thoughts
Pelvic Congestion Syndrome is a complex condition that isn’t easy to diagnose. Once identified, there are many effective medical treatments to alleviate pain and discomfort. If you are experiencing pelvic pain that has troubled you for more than six months, it may be time to contact a vascular specialist. It is not a lethal or life-threatening disease, but it still warrants medical attention.
Dealing with chronic pain isn’t an easy task and may lead to disruptions in daily life. Rest assured that there are effective treatments available and your doctor will guide you in taking the necessary steps to stay healthy, maintain wellness, and establish peace of mind. You and your vascular specialist can create a personalised treatment plan to combat Pelvic Congestion Syndrome.
Frequently asked questions
Pelvic Congestion Syndrome is associated with restricted blood flow in the pelvic area. When the body changes during pregnancy, the veins may be damaged. The veins may lead to malfunctioning organs which can affect fertility. Dysfunctional pelvic veins do not close properly, causing backflow and interruption of bodily functions. This condition causes chronic pelvic pain since the twisted veins cannot handle the sudden onset of blood. See “What causes Pelvic Congestion Syndrome” section above for a detailed explanation.
Signs and symptoms (Pelvic pain, varicose veins, digestive problems, stress incontinence, and haemorrhoids) often interfere with daily activities such as work, school, and hobbies. See “What are the various signs and symptoms of Pelvic Congestion Syndrome?” section above for a detailed explanation. Aside from the other signs, one may also experience mental health problems such as anxiety and depression. Pelvic Congestion Syndrome causes women to experience fertility problems. There is a chance that the affected and damaged veins may cause the reproductive organs (uterus, ovaries, and fallopian tubes) to malfunction. Pain during sexual intercourse is a symptom, which makes it difficult for women to conceive properly.
Pelvic Congestion Syndrome can be diagnosed using a CT scan, pelvic venogram, ultrasound, laparoscopy, and blood & urine tests. The specific method of diagnosis may differ among medical professionals. (See “How can Pelvic Congestion Syndrome be diagnosed?” for an in-depth look into various methods for diagnosis)
Pelvic Congestion Syndrome can be treated through surgical and non-surgical management. Surgical management includes open surgical methods such as salpingo-oophorectomy and hysterectomy. Non-surgical management includes anti-inflammatory drugs, hormonal medications, and alternative therapies such as physical therapy and acupuncture. Pelvic and Ovarian Vein Embolisation Surgery is another potential treatment for this condition. It is a minimally invasive procedure that uses a catheter, fluoroscopy, and tiny titanium coils to seal damaged veins. After these treatments, it is expected that the patient will experience less pain and discomfort. See “What should I expect after I get treated for Pelvic Congestion Syndrome?” for more information.
75% of patients who undergo Pelvic and Ovarian Vein Embolisation Surgery experience relief from the pains and discomfort associated with the condition. This condition is not a lethal or life-threatening disease, but it is the type of condition that calls for medical intervention. Patients who undergo treatment are expected to feel relief from the symptoms of Pelvic Congestion Syndrome.
References:
- https://flo.health/pregnancy/pregnancy-health/pains-and-discomforts/pelvic-congestion-syndrome
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/pelvic-pain
- https://www.sgvascularctr.com/service/pelvic-congestion-syndrome/
- https://my.clevelandclinic.org/health/diseases/24213-pelvic-congestion-syndrome
- https://www.topdoctors.co.uk/medical-articles/pelvic-congestion-syndrome-symptoms-diagnosis-and-treatment
- Tags:
- chronic pelvic pain treatment
- congested pelvic
- pelvic congestion causes
- pelvic congestion clinic Singapore
- pelvic congestion complications
- pelvic congestion diagnosis
- pelvic congestion management
- pelvic congestion outpatient care
- pelvic congestion patient education
- pelvic congestion risk factors
- pelvic congestion specialist
- pelvic congestion surgery
- pelvic congestion symptoms
- pelvic congestion syndrome
- pelvic congestion syndrome Singapore
- pelvic congestion syndrome specialist near me
- pelvic congestion therapy
- pelvic congestion treatment
- pelvic pain Singapore
- pelvic vein disorder
- pelvic vein embolization
- pelvic vein issues
- vascular pelvic health
