
Image source: [https://www.victorianvascular.com.au/home/arterial-disease/peripheral-arterial-disease/]
Peripheral Artery Disease (PAD) is a condition in which the blood vessels supplying the arms and/or legs are narrowed leading to reduced supply of oxygen and nutrients to these areas. Symptoms of PAD can range from aching or cramps in the affected limb to wounds or gangrene, ultimately resulting in amputation of the affected arm or leg.
There is an increasing frequency of PAD, especially in Singapore where diabetes mellitus (one of the leading causes of PAD) is becoming more and more prevalent, with about 1 in 10 adults having diabetes as of 2017. Up to a quarter of diabetics will develop foot wounds/ulcers in their lifetime, and with a 10-fold increased risk of having a lower limb major amputation as opposed to a non-diabetic. Singapore has the unfortunate accolade of having one of the highest rates of leg amputations amongst the developed countries, with approximately 3-4 amputations performed daily nationwide.
What is Peripheral Artery Disease?
Peripheral Artery Disease (PAD) is characterized by narrowing or blocking of the arteries that supply blood to the limbs, most commonly the legs. This is due to atherosclerosis, a disease in which there is plaque buildup within the artery walls. This decreases the amount of blood that can reach the affected area, resulting in symptoms like leg pain, weakness, and numbness when exercising.
Atherosclerosis (plaque buildup in the wall of the artery) first starts when the walls of the arteries become damaged and inflamed (usually due to diseases such as hypertension and diabetes or due to ageing). This artery wall damage leads to a buildup of fat and inflammatory cells in the vessel wall, which triggers an inflammatory chain reaction. Plaque rupture eventually occurs, causing platelet adhesion and further progression of the atherosclerotic plaque. The artery’s lumen is gradually narrowed over months to years thus decreasing blood flow within the blood vessel and causing symptoms of PAD.
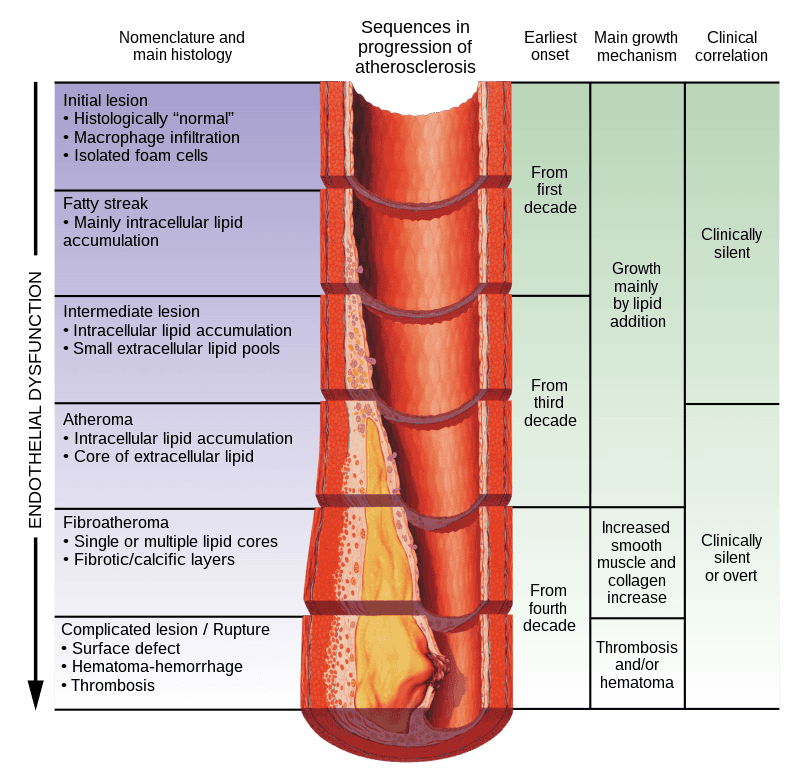
Image source: [https://en.wikipedia.org/wiki/Atherosclerosis]
The Rutherford classification is one of the methods utilized by doctors to classify and document the severity of PAD. It is also useful to guide appropriate treatment of the disease. The Rutherford classification categorizes the symptoms of PAD from 0 to 6 with increasing severity as the category level increases. In general, category 0-2 cases can be managed with lifestyle modification and medications to reduce the risk factors of PAD. In category 3-6 cases, medications frequently are unable to achieve adequate symptom control, and surgery will be required to improve the blood supply to the affected limb. This is especially true for category 4-6 cases which are collectively termed critical limb ischemia, and in which there is a significant risk of amputations.
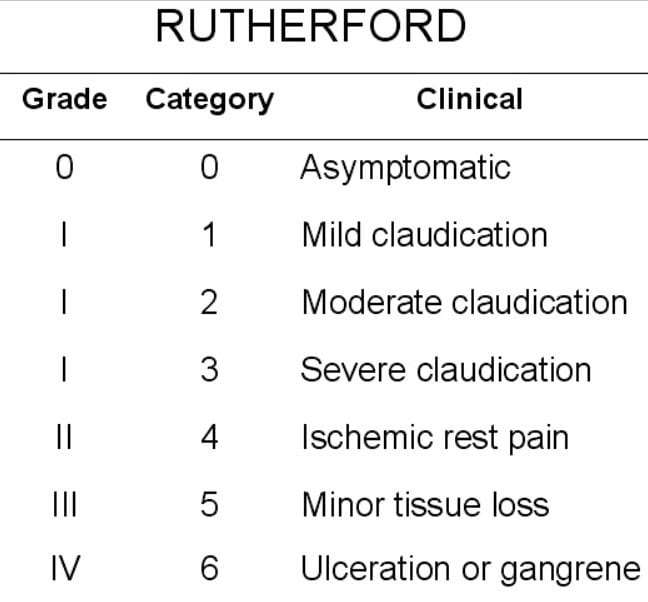
Image source: [www.wikidoc.org/index.php/Peripheral_arterial_disease_classification]
It is important to emphasize that the earlier treatment is initiated for PAD, the better the outcomes. The risk of unsuccessful treatment increases as the category level increases. This is especially true for category 4-6 cases (critical limb ischemia), where even a delay of a couple of days in seeking medical treatment may result in extensive, irreversible gangrene and an unsalvageable leg.
What are the Causes and Risk Factors of Peripheral Artery Disease?
Peripheral Artery Disease (PAD) can be caused by a variety of factors, including blood vessel inflammation (vasculitis), direct injury to the vessel from trauma, or radiation exposure; but by far the most common cause of PAD is atherosclerosis (plaque buildup in the wall of the artery).
Risk factors for the development of atherosclerosis include:
- Smoking/tobacco use – The chemicals in cigarette and other forms of tobacco smoke disrupts the normal lipid metabolism, thus promoting fatty deposits in the artery walls. The chemicals also have a direct effect on the blood vessel inner lining (endothelium), smooth muscle cells and the macrophages (specialized white blood cells), all of which act together to promote atherosclerosis.

Image source: [https://en.wikipedia.org/wiki/Smoking]
- Diabetes mellitus – Diabetes promotes the development of atherosclerosis by disrupting platelet aggregation and causing endothelium and smooth muscles cell dysfunction. It predominantly affects the smaller blood vessels below the level of the knee (microvascular disease) and significantly increases the risk of an amputation.
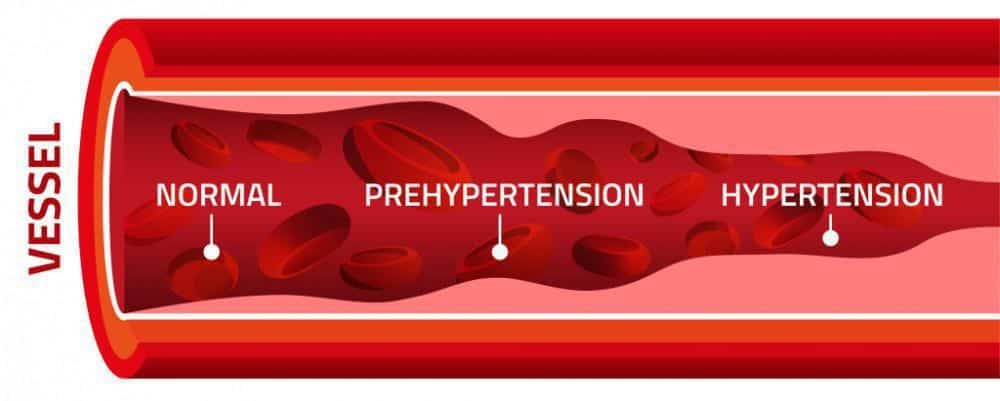
Image source: [https://www.sprucemedicalgroup.com/blog/when-to-initiate-treatment-for-borderline-hypertension]
- Hypertension (high blood pressure) – Poorly controlled blood pressure damages the arteries and increases the risk of atherosclerosis. A target blood pressure of less than 130/85mmHg is recommended to reduce the risk of PAD.
- High blood cholesterol – Elevated levels of the “bad” LDL-cholesterol are associated with an increased risk of atherosclerosis. Guidelines recommend reducing LDL-cholesterol levels to <70mg/dl which can be achieved by compliance with dietary modifications and medications.
There are also some non-modifiable risk factors for the development of atherosclerosis such as age (increased risk in people aged >65 years old) as well as genetics (risk is higher in individuals with a family history of the disease).
What are the Dangers (complications) of Peripheral Artery Disease?

Image source: [https://www.scientificamerican.com/article/new-approach-to-amputation-could-reduce-phantom-pain/]
Peripheral artery disease (PAD) can lead to various complications ranging from mild muscle discomfort when walking (claudication) to severe gangrene, ulcers, and the need for limb amputation. The earlier treatment is initiated for PAD, the better the outcomes, and the higher the chance of avoiding an amputation of the toes, feet or even the entire leg. In severe late-stage PAD with extensive tissue gangrene, the superimposed bacterial infection and the toxins released from the dying tissue ultimately leads to mortality.
How can I know if I have Peripheral Artery Disease (Signs/Symptoms/Diagnosis)?
Some patients may not have any signs or symptoms in the early stages of PAD, however guidelines from the Ministry of Health (Singapore) still recommend screening for the presence of “silent” PAD especially in individuals with risk factors (detailed above in “What are the Causes and Risk Factors of Peripheral Artery Disease?”). Even without any symptoms, the presence of PAD is usually an indication of global (whole body) atherosclerosis, which if not treated, can increase the risk of stroke, heart attack and cardiovascular death. Screening for PAD in individuals without any signs or symptoms involves:
- Checking the foot for any ulcers or callosity (areas of thickened skin)
- Checking for the presence and quality of the distal foot pulses (the dorsalis pedis and the posterior tibial pulses)
- Doing a monofilament test for sensation in the foot
- Doing a test for the amount of blood flow in the foot arteries (ankle brachial pressure index, ABPI and toe brachial index, TBI)
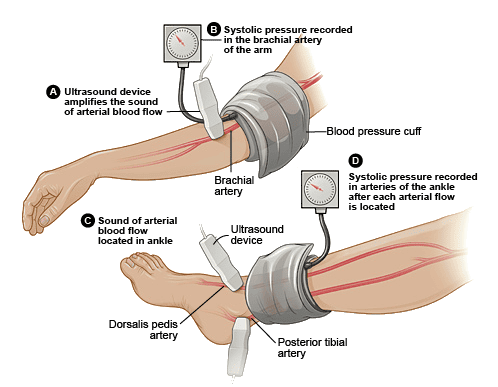
Image source:
[https://www.cuh.nhs.uk/our-services/surgery/vascular-studies-unit/pre-and-post-exercise-abpi-walkingtreadmill-test/]
If the presence of PAD is detected, treatment to mitigate the various risk factors should be initiated, even if the person has no symptoms. The aim is to prevent the progression of PAD, prevent limb amputations and reduce the risk of stroke and heart attacks.
As the severity of PAD progresses, early signs and symptoms which may start to appear include:
- Claudication – This is an aching pain in the muscles of the legs (buttocks, thighs, calves) when walking/running. It is a sign that there is insufficient blood supply to these muscles resulting in reduced oxygen supply and impaired clearance of metabolic waste from the legs.
- Rest pain – Pain in the feet and toes when resting on the bed can be a sign of significant PAD affecting the blood flow to the foot. This pain is typically relieved by hanging the leg down by the side of the bed, as this position utilizes gravity to help pull the blood down the leg.
- Skin changes – People with significant PAD typically have poorer quality skin due to the reduced blood flow to the area. Some skin changes which may be observed include loss of hair, thinned out dry skin and dystrophic nails.
- Wounds and ulcers – PAD significantly reduces the blood flow to the leg thus affecting both the delivery of oxygen and nutrients to the tissues, and the removal of metabolic waste products from the area. This results in poor quality skin, which is quick to injure and slow to heal, thus resulting in recurrent wounds and ulcers. These wounds can form even from minor injuries such as from a tight-fitting shoe or from a stubbed toe.
- Gangrene – Gangrene is irreversible death of tissue. This is observed in late-stage PAD when there is complete absence of blood flow to an area of the leg or foot resulting in the tissue completely dying and turning black (gangrene). Gangrenous tissue should be removed as it is highly prone to bacterial infection.
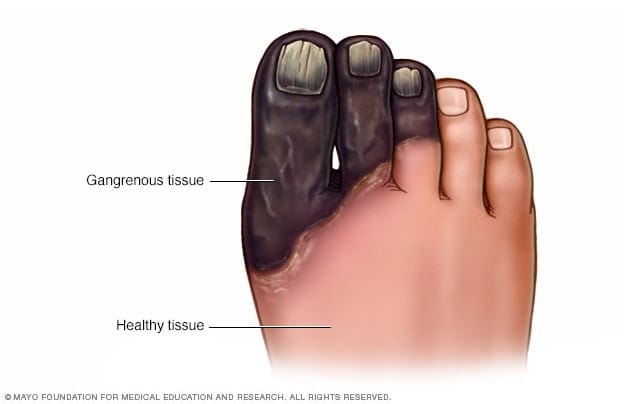
Image source: [https://www.mayoclinic.org/diseases-conditions/gangrene/symptoms-causes/syc-20352567]
The diagnosis of PAD first involves a scan to investigate the major arteries in the leg, looking for areas of reduced blood flow, narrowing and/or blockage. The methods used to scan the leg arteries include either doppler ultrasound, computer tomography (CT scan) or catheter angiography. A doppler ultrasound is typically the first-choice option as it does not involve any radiation and does not require the injection of a special dye (contrast) into the blood stream, which may damage the kidneys. Other tests that may be performed for people with PAD include tests looking at fitness for surgery (ECG, chest X-ray etc.) and tests looking for signs of infection (blood white cell count, foot MRI scan etc.)
How can I prevent myself from getting Peripheral Artery Disease?
There are modifiable and non-modifiable risk factors that contribute to PAD development, and tackling the modifiable risk factors such as smoking, diabetes, high blood pressure and high cholesterol can significantly reduce the risk of developing PAD (see “What are the Causes and Risk Factors of Peripheral Artery Disease?” section above for more details).
Optimal control of diabetes, high blood pressure and high cholesterol can be achieved by adhering to a healthy balanced diet rich in fruits and vegetables and low in salt, refined carbohydrates, and fats. It is critical to take all medications prescribed religiously and attend the regular doctor appointments to ensure the diseases are properly treated and to adjust the medications and diet if necessary.

Image source: [https://www.facebook.com/153581836497236/photos/a.158632552658831/235606354961450/?type=3]
General advice of regular exercise, maintaining a healthy body weight (BMI between 18 to 25) and stopping any smoking/tobacco use can not only reduce the risk of PAD, but also improve overall health and reduce risks of many other diseases such as cancers, strokes, and heart attacks.
How can I prevent an amputation if I have Peripheral Artery Disease (PAD)?
Once PAD has developed, it is crucial to adhere strictly to lifestyle and dietary advice, as well as take all necessary medications to prevent the progression of the disease. The lifestyle and medical advice given above (“How can I prevent myself from getting Peripheral Artery Disease?”) also applies to people with established PAD.
Additional factors to pay attention to, in order to prevent an amputation, include footwear and footcare modifications. People with longstanding diabetes typically have reduced sensation in the feet (due to nerve damage from the diabetes), and they may not be aware of minor cuts/bruises sustained from accidental injury or ill-fitting shoes. If these minor injuries are not cleaned and dressed properly, they may get infected and progress to large wounds/gangrene thus leading to amputations. People with PAD should avoid ill-fitting shoes which can cause callosities or abrasions to the feet, and they should inspect the feet on a daily basis for any wounds. In those with advanced PAD, it is advisable to have a regular review of their foot condition with a trained podiatrist.

Image source:
[https://www.healthxchange.sg/diabetes/essential-guide-diabetes/diabetes-foot-care-how-choose-shoes-good-support-fit]
Besides the medications to control the risk factors (such as diabetes, high blood pressure, and high cholesterol) patients with PAD may also be prescribed a “blood-thinning” medication by their doctor. These are a group of medications which suppress the ability of the body to form clots, and they have been shown to significantly reduce the risk of progression of PAD, reduce risk of amputations, and reduce risk of stroke and heart attacks. These “blood-thinning” medications are not for everyone, as the benefits have to be weighed against the risks of the increased bleeding potential, and they should only be used under the guidance of a doctor.
Once PAD has progressed to cause significant blockage of the major blood vessels in the leg, surgery may be necessary to restore blood flow to the foot and avoid an amputation. This is especially critical once the patient starts experiencing signs of critical limb ischemia, namely pain in the foot even when lying in bed or the development of ulcers and/or gangrene. Early consultation with a Vascular specialist can improve the chances of a successful revascularization surgery (surgery to restore the blood flow to the foot), and the avoidance of an amputation. Most times, surgery can be performed via a minimally invasive (“key-hole”) approach under sedation, thus significantly reducing the risks of the operation, with minimal down-time and faster recovery.
Can Peripheral Artery Disease (PAD) be treated without surgery?
PAD can be managed without surgery in the early stages, namely Rutherford categories 0-3 (see above “What is Peripheral Artery Disease?” for an explanation of the Rutherford categories). Once PAD has progressed beyond Rutherford 3 (i.e. develop rest pain or ulcers/gangrene) surgery becomes necessary to prevent amputation of the leg.
The non-surgical management of early-stage PAD involves treating any risk factors such as smoking and diabetes, as well as observing good footwear and footcare habits (please see “How can I prevent myself from getting Peripheral Artery Disease?”and “How can I prevent an amputation if I have Peripheral Artery Disease (PAD)?”for more details).
Targeted non-surgical treatment for claudication symptoms (pain when walking) associated with PAD include:
- Blood vessels dilators such as Cilostazol – These medications work by causing the blood vessels in the leg to dilate (increase in size) and accommodate more blood flow through their channels. The moderate increase in blood flow can help compensate for some of the arterial blockage caused by PAD.
- A supervised exercise program is another non-surgical option that can help improve symptoms of claudication. A typical program involves walking on a treadmill in a supervised setting at least three times per week using the “Start/Stop” exercise: walk until the discomfort reaches a moderate level, then stop, wait until the discomfort subsides completely, and then resume walking.
When would my doctor recommend surgery for Peripheral Artery Disease?
Patients with a Rutherford category of 4–6 (see above “What is Peripheral Artery Disease?” for an explanation of the Rutherford categories) typically require surgery to restore blood flow in their affected limbs to avoid a major amputation. Surgery may also be considered for some patients with Rutherford category 3 PAD, especially if the symptoms are significant to impact lifestyle, or if there is no improvement after a trial of non-surgical management (see above “Can Peripheral Artery Disease (PAD) be treated without surgery?” for non-surgical management of PAD).
What surgical options are there for Peripheral Artery Disease (PAD)?
Surgery for PAD can be either open or endovascular (i.e. minimally invasive “key-hole”) surgery. Open surgery encompasses:
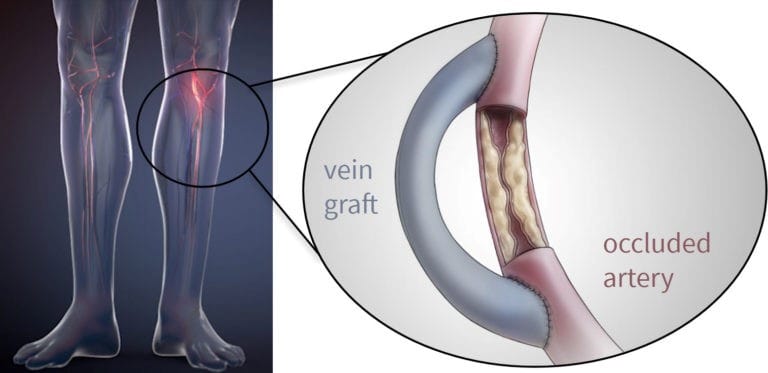
Image source: [http://ntxvascular.com/surgical-bypass/]
- Bypass surgery – a prosthetic (plastic) tube graft or a harvested vein graft is attached from a proximal healthy segment of the artery to a distal healthy part of the artery, thus allowing blood to flow to the foot and bypassing the blocked arterial segment affected by PAD.
- Endarterectomy surgery – the segment of diseased artery affected by PAD is opened and the atherosclerotic plaque removed. The artery is then repaired using a patch of prosthetic or vein material.
Endovascular surgery involves a small 5-10mm incision in the skin through which various equipment such as wires, balloons and stents are introduced to treat the blocked or narrowed segment of artery. Endovascular surgery has the added advantage of lower operative risk, minimal scarring and quicker recovery as compared to open surgery, albeit with a slightly higher risk of recurrence of the disease requiring a repeat procedure in some cases.
All you need to know about Endovascular Surgery for Peripheral Artery Disease (PAD)
Endovascular surgery was first pioneered in 1964 by an American interventional radiologist (Dr Charles Dotter). It has improved over the years with technological advances in wire, balloon and stent technology, and is now able to provide more than 90% technical success rate at opening any narrowed or blocked leg artery. Recent studies have shown that endovascular surgery can achieve comparable near-term results when compared with open surgery, and with the added advantage of lower operative risks, less scarring and quicker recovery. There are instances where open surgery may be a better option (e.g. such as in atherosclerosis involving the artery at the groin, the common femoral artery), and your specialist should be able to advise you on the most appropriate operation for your condition.
In endovascular surgery, a small 5-10mm incision is made in the skin through which various equipment is introduced to treat the blocked or narrowed segment of artery. During the operation, the equipment is guided by use of fluoroscopy (specialized X-rays) and a special dye (iodinated contrast) which is injected into the blood stream to help visualize the artery. Endovascular operations thus need to be performed in specialized operating theatres which are lead-lined (to prevent radiation leak) and with a C-arm for fluoroscopy. Such specialized operating rooms are usually termed hybrid operating theatres.
The equipment used during endovascular surgery include:

Image source:
- Sheaths – These are long narrow tubes which are placed through the skin and into the artery via which all the other devices pass through. They come in various sizes and lengths and are removed at the end of the operation.
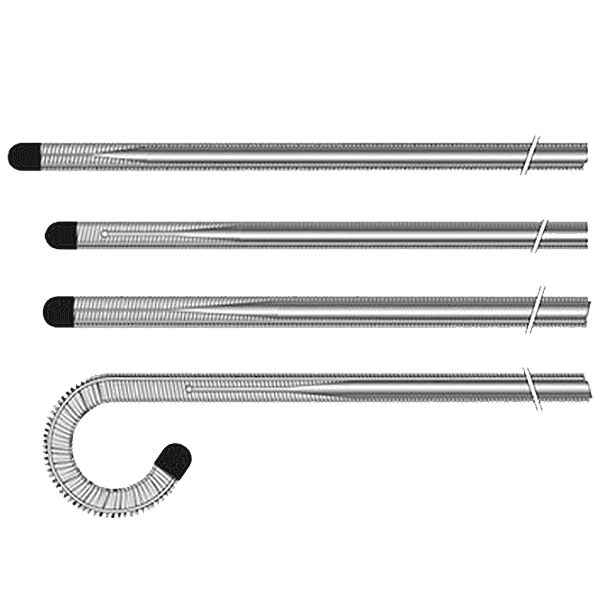
Image source: [https://www.bostonscientific.com/en-US/products/guidewires/starter-guidewire.html]
- Wires – These are akin to the railroads over which the other devices pass along to reach the target lesion. They come in various sizes, lengths and stiffness, and must be passed under X-ray guidance across the arterial lesion to be treated.
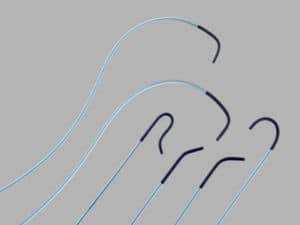
Image source: [https://vascularnews.com/beacon-tip-catheters-available-in-europe-again/]
- Catheters – Catheters are long narrow tubes which are passed over wires to aid in their movement within the vessel. Medications that dissolve clots or cause artery dilatation can also be infused into the vessel via these catheters.
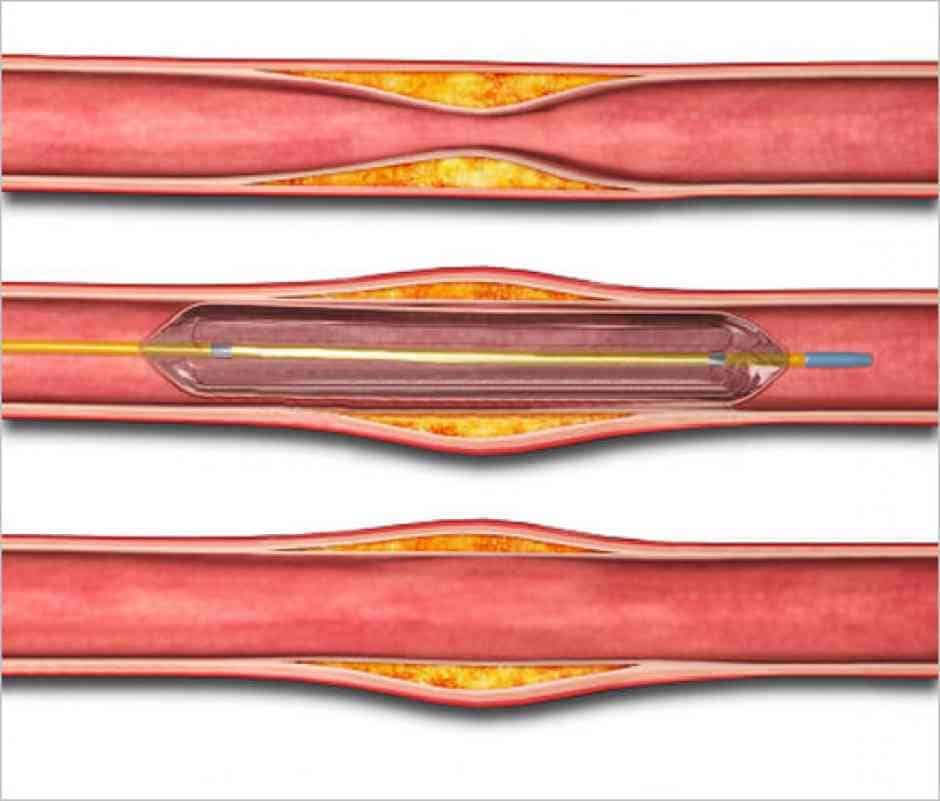
Image source: [https://www.conicvascular.com/balloon-angioplasty]
- Balloons – After a wire has been passed across the target lesion, various diameter and length balloons can then be tracked along the wire and inflated to open the narrowed/blocked artery. The balloons are sometimes coated with medication which can reduce the risk of recurrence of the atherosclerotic plaque. The balloon is deflated and removed at the end of the procedure.
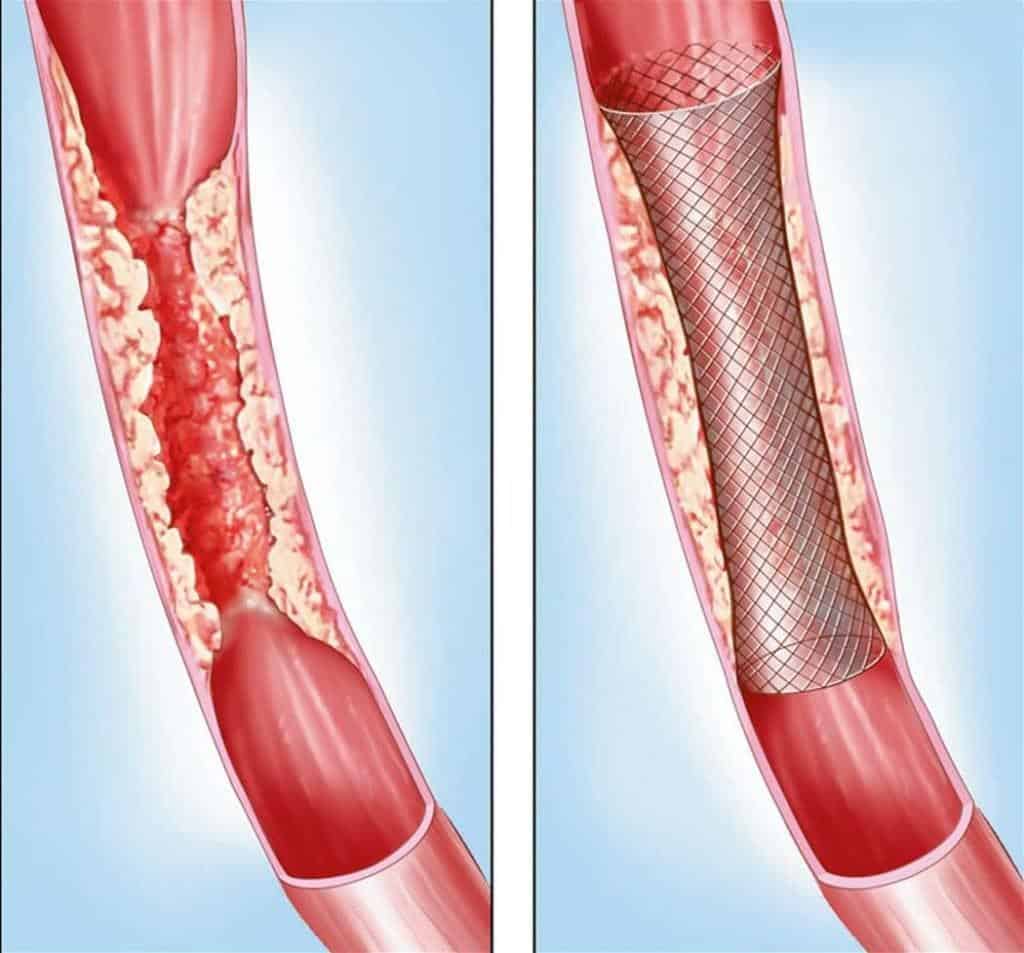
Image source: [https://www.vascularsurgeryassociates.net/contents/treatments/stenting]
- Stents – Occasionally, the atherosclerotic plaque is very bulky and narrows the artery lumen almost immediately after the balloon is deflated. In such instances, a stent (wire mesh-like tube) can be inserted to keep the lumen open. The stent remains in the vessel and is not removed.
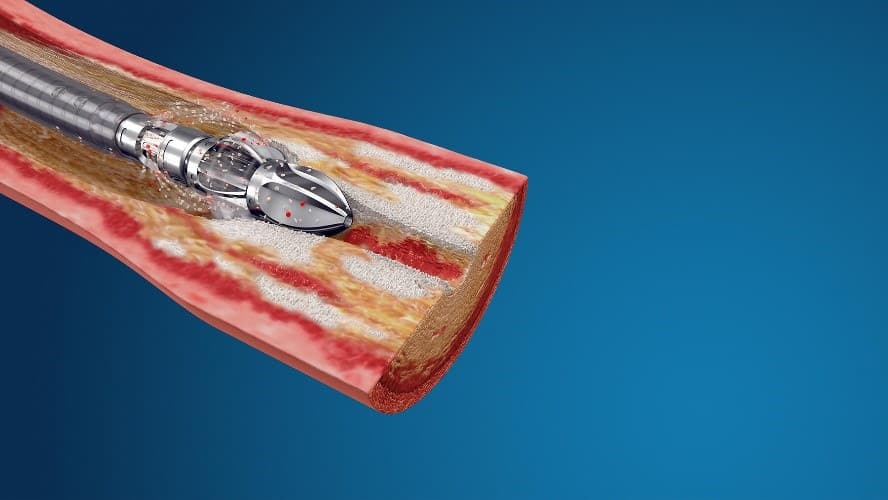
Image source: [https://www.bostonscientific.com/en-EU/products/atherectomy-systems/jetstream-atherectomy-system.html]
- Atherectomy/thrombectomy devices – Specialized devices which can extract out atheroma or clots are occasionally used for very severe cases.
As with any medical procedure, there are risks involved with the operation. Risks associated with endovascular surgery for PAD may include access site bleeding or pseudoaneurysms (weakening of the wall of the artery), dissections (damage to the inner lining of the vessel) or thrombus (clot) formation in the artery, and contrast-induced nephropathy (a type of kidney damage caused by the dye used during the procedure). Technical failure can also occur, in which case open surgery may be required.
Overall, results from endovascular surgery for PAD are comparable to conventional open surgery, with a lower risk of complications and quicker recovery times. It is not to say that open surgery has become obsolete as there are some instances, such as very long segment occlusions, which may benefit more from open surgery, thus it is important to discuss all options with a specialist trained in both approaches to decide which surgery is more suitable for your disease process.
What is recovery like after endovascular surgery for Peripheral Artery Disease (PAD)?
Patients with peripheral artery disease (PAD) who undergo endovascular surgery can expect a quick recovery with minimal risk of complications. Immediately after the procedure, the patient will need to lie flat with a bandage applied to the groin incision site and be monitored in a recovery facility for a few hours. The bandage is eventually removed, and the groin incision site is checked for any signs of bleeding before the patient can be discharged home.
It is important to drink plenty of water and remain well hydrated for the next 48h to prevent injury to the kidneys from the dye used during the operation. “Blood-thinning” medications are typically prescribed for at least 6 months to prevent early recurrence of the artery blockage. The patient will be advised to do light activities for the next 2 weeks and resume full activities thereafter.
What can I do to avoid the recurrence of Peripheral Artery Disease?
Image source:
[https://www.emergency-live.com/health-and-safety/anticoagulants-what-they-are-and-when-they-are-essential/]
After surgery for PAD, adherence to lifestyle and dietary modifications targeting the risk factors associated with PAD, can significantly reduce the risk of recurrence of the disease (see above section “How can I prevent myself from getting Peripheral Artery Disease?” for details). Taking the “blood-thinning” medications such as Rivaroxaban or Clopidogrel can also contribute to the prevention of PAD recurrence. Of utmost importance is to attend regular medical appointments and seek medical attention urgently in the event rest pain, ulcers or gangrene occur. The earlier treatment is initiated for recurrent PAD, the better the chances of good outcomes and avoidance of a major amputation.
Conclusion and personal comments
Peripheral arterial disease is increasing in frequency in Singapore, mainly due to the increased incidence of diabetes. It is a debilitating disease which if not treated early, can lead to irreversible gangrene and ultimately lower limb major amputations. The good news is that advancement in technology has allowed surgeons to treat more than 90% of such cases via a minimally invasive endovascular approach. Endovascular surgery has been a game-changer, allowing PAD to be treated under local anesthetic and in many cases as a day surgery procedure, allowing even very frail patients with multiple medical conditions to benefit from surgery and avoid a major amputation.
Frequently Asked Questions:
· PAD refers to the condition whereby narrowing or blockage of arteries occur, mainly due to build-up of atheromatous plaques
· This artery narrowing impedes blood supply to the foot, thus leading to leg pain, weakness, numbness, wounds, gangrene and even amputations.
· See “What is Peripheral Artery Disease?” section above for more details.
· Peripheral Artery Disease (PAD) can be caused by a variety of factors, including blood vessel inflammation (vasculitis), direct injury to the vessel from trauma, or radiation exposure; but by far the most common cause of PAD is atherosclerosis (plaque buildup in the wall of the artery).
· Risk factors for the development of atherosclerosis include:
1. Smoking/tobacco use
2. Diabetes mellitus
3. Hypertension (high blood pressure)
4. High blood cholesterol
5. Increasing age (increased risk in people aged >65 years old)
6. Genetics (risk is higher in individuals with a family history of the disease)
· See “What are the Causes and Risk Factors of Peripheral Artery Disease?” section above for more details.
· Symptoms of PAD can range for mild claudication (pain when walking) to serious ulcers, gangrene and ultimately amputation of the leg.
· PAD is also a marker for increased risk of stroke, heart attack and cardiovascular related mortality.
· See “What are the Dangers (complications) of Peripheral Artery Disease?” section above for more details.
· In the early stages, PAD may exhibit no signs/symptoms and can only be detected by a screening test such as the ankle brachial pressure index (ABPI) test.
· As the disease progresses, the person may develop signs of claudication. This is an aching pain in the muscles of the leg (buttocks, thighs or calves) when walking a certain distance.
· Late manifestations of the disease include ulcers and tissue gangrene.
· See “How can I know if I have Peripheral Artery Disease (Signs/Symptoms/Diagnosis)?” section above for more details.
• Treatment for PAD begins with lifestyle changes such as quitting smoking, increasing physical activity, and maintaining a healthy diet.
• For diabetics, it is important to keep the blood sugar levels under tight control with diet and medications. For hypertensives, take the necessary medications to maintain blood pressure within the normal range (less than 140mmHg systolic and less than 90mmHg diastolic). For patients with high cholesterol, adhere to a low fat, high fiber diet and take all prescribed medications.
• For most patients, starting a “blood-thinning” medication such as Rivaroxaban or Clopidogrel can help prevent disease progression and reduce risk of strokes and heart attacks.
• Surgery (either open or endovascular) will be necessary to restore blood flow in patients with critical limb ischemia, so as to avoid a leg amputation.
• See “Can Peripheral Artery Disease (PAD) be treated without surgery?” section above for more details.
PAD can be managed without surgery in the early stages, but once PAD has progressed beyond Rutherford 3 (see above “What is Peripheral Artery Disease?” for an explanation of the Rutherford categories) surgery becomes necessary to prevent amputation of the leg.
The non-surgical management of early-stage PAD involves treating any risk factors such as smoking and diabetes, as well as observing good footwear and footcare habits (please see “How can I prevent myself from getting Peripheral Artery Disease?” and “How can I prevent an amputation if I have Peripheral Artery Disease (PAD)?” for more details).
Targeted non-surgical treatment for claudication symptoms (pain when walking) include blood vessels dilators such as Cilostazol and a supervised exercise walking program.
See “Can Peripheral Artery Disease (PAD) be treated without surgery?” section above for more details.
There is no best treatment option for Peripheral Artery Disease/Peripheral Arterial disease (PAD) in Singapore however, the treatment will depend on individual circumstances and disease severity. Early intervention with lifestyle changes and medications can be effective for mild cases, while more severe cases may require surgical intervention.

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- arterial vein disease Singapore
- best treatment for peripheral artery disease Singapore
- PAD blood flow
- PAD causes
- PAD complications
- PAD exercise recommendations
- PAD lifestyle changes
- PAD management
- PAD outpatient care
- PAD pain relief
- PAD patient education
- PAD prevention tips
- PAD risk factors Singapore
- PAD specialist Singapore
- PAD surgery Singapore
- PAD symptoms
- PAD therapy
- pad treatment singapore
- PAD vascular health
- peripheral arterial disease singapore
- peripheral arterry disease Singapore
- peripheral artery blockage
- peripheral artery disease
- peripheral artery disease diagnosis
- peripheral artery disease Singapore
- peripheral artery disease treatment
- Peripheral Vascular Disease
