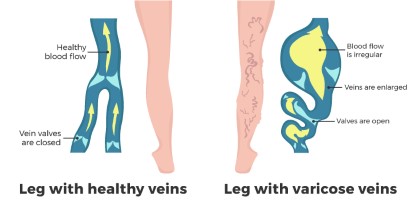
Veins transport deoxygenated blood back to the heart. In the legs, blood initially gathers in the superficial veins, located just beneath the skin, and is then directed into deeper veins running through the calf muscles. The contraction of the calf muscles plays a crucial role in propelling the blood upward against gravity. To ensure blood flows in the right direction, one-way valves inside the veins prevent backflow. When these valves malfunction, blood accumulates in the superficial veins, causing them to expand and develop a twisted and darkish-blue appearance, a condition known as varicose veins.
(image source: https://coremedicalwellness.com/varicose-veins-vs-spider-veins/)
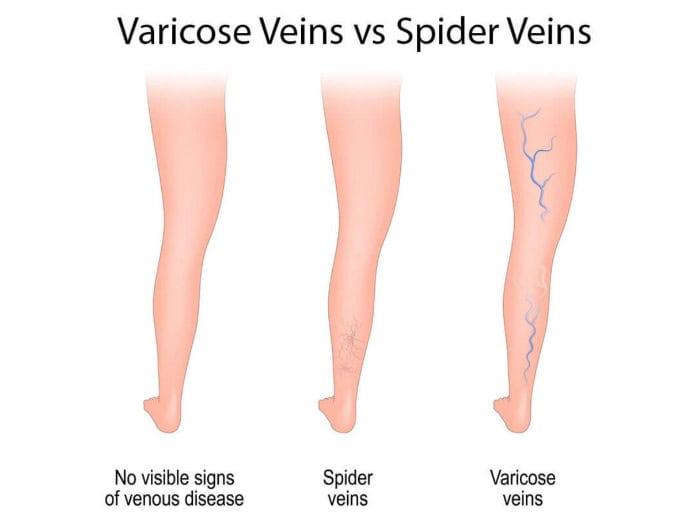
The Difference Between Spider Veins and Varicose Veins
Spider veins share similarities with varicose veins. Spider veins are smaller and situated closer to the skin’s surface. They typically appear as red or blue patterns resembling tree branches or spider webs. Spider veins are commonly found on the legs or face and can cover either a small or large area. Spider veins are visible beneath the skin but do not cause the skin to bulge, unlike varicose veins.
Varicose veins are twisted veins that can appear in shades of blue, red, or skin-colored. The larger veins may take on a ropelike appearance and cause the skin to protrude. Varicose veins typically occur on the thighs, the front and back of the calves, or the inner parts of the legs near the ankles and feet. During pregnancy, varicose veins can develop in areas such as the inner thighs, lower pelvic region, and buttocks.
The Formation of Varicose Veins
Let’s explore the gradual progression that leads to the formation of varicose veins, uncovering the key factors and mechanisms at play:
- Under normal conditions, blood in the veins of the legs flows towards the heart, aided by one-way valves in the veins.
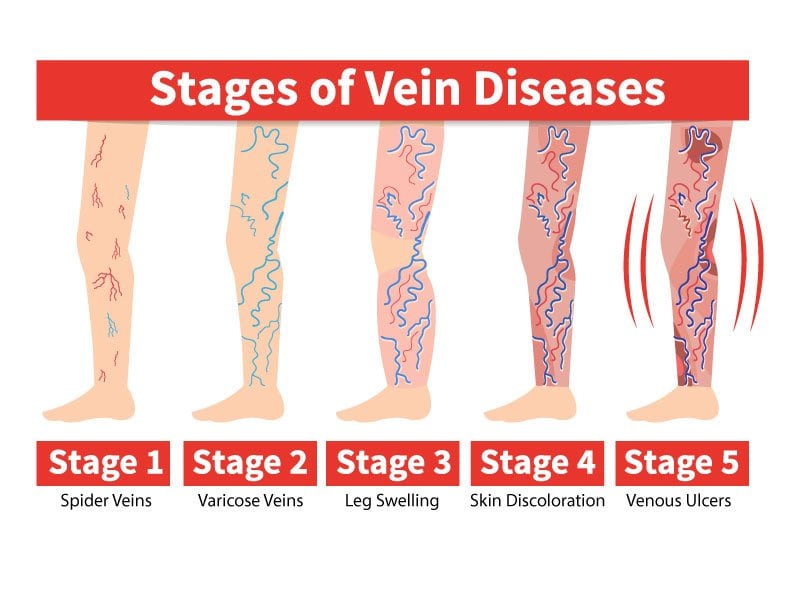
- Varicose veins develop when these one-way valves in the superficial veins near the skin’s surface become weakened or damaged. This can occur due to various factors, including genetics, hormonal changes, and aging.
- As the valves weaken, they fail to prevent blood from collecting or pooling in the veins, primarily in the legs. This accumulation of blood causes the veins to become enlarged.
- Prolonged periods of sitting or standing can exacerbate the condition. Inactivity or immobility can lead to blood pooling in the leg veins, resulting in increased pressure within these veins. The heightened pressure inside the veins can cause them to stretch and become elongated.
This stretching can weaken the walls of the veins and further damage the already compromised valves. The combination of weakened valves, blood accumulation, increased pressure, and vein stretching results in the characteristic appearance of varicose veins—twisted and often bluish or reddish in color.
(image source: https://www.physiciansveinclinics.com/blog/the-stages-of-vein-disease)
Common Risk Factors Associated with Varicose Veins
- Age – Varicose veins become more prevalent as individuals age. Over time, the valves in the veins can wear out, which hinders their ability to prevent blood from flowing backward. This valve dysfunction can lead to blood pooling in the veins, contributing to the development of varicose veins.
- Gender – Varicose veins are more frequently observed in females. This is partly due to hormonal changes that occur during pregnancy, pre-menstruation, and menopause. These hormonal fluctuations can relax the walls of the veins, making them more susceptible to becoming varicose.
- Pregnancy – Pregnancy brings about several physiological changes, including an increase in the volume of blood in the mother’s body to support the growing fetus. To accommodate this heightened blood volume, the veins expand, and the added pressure can lead to the development of varicose veins in the legs.
- Family History – Family history plays a significant role in the likelihood of developing varicose veins. Individuals with a strong family history of varicose veins are at a higher risk of experiencing the condition themselves. Genetic factors can influence the integrity of vein valves and overall vein health.
- Obesity – Being overweight or obese places additional pressure on the veins, especially in the lower extremities. Excess body weight can impede proper blood flow in the veins and exacerbate the risk of varicose veins.
Standing for Prolonged Periods – Occupations or activities that require prolonged periods of standing can lead to poorer blood flow in the leg veins. When you stand for extended durations, it can be more challenging for blood to circulate efficiently, potentially contributing to varicose vein formation.
(image source: https://www.whattoexpect.com/pregnancy/pregnancy-health/best-home-remedies-varicose-veins-pregnancy/)
Understanding the Link Between Pregnancy and Varicose Veins
Varicose veins during pregnancy can be attributed to several factors. Hormonal changes also affect the circulatory system. The growth of the baby places increased pressure on blood vessels in the pelvis. The blood flow in both the pelvic region and the legs can increase, leading to increased blood pressure as your body adjusts to the pregnancy. Furthermore, the overall increase in blood volume in the body during pregnancy exacerbates the situation. These combined forces make it challenging for blood to flow against gravity from the legs back to the heart.
Whether you have varicose veins or if you are at risk of developing this condition, it is important to take note of the following symptoms:
- Swollen and enlarged networks of red, purple, or blue vessels
- A persistent sensation of heaviness or swelling in your legs
- Aching in your legs
- Skin discoloration or darkening around the veins
- Itchy skin around the veins
If you experience these symptoms, it is best to contact a vascular surgeon. They can investigate the issue, provide advice, and help you decide on a treatment plan. It’s all about taking care of your vascular health for your long-term wellbeing.
The Importance of Vascular Surgeons in Treating Vascular Conditions in Singapore
Vascular surgeons aim to provide methods for screening, diagnosis, and treatment for patients with varicose veins. With the combined results from a clinical physical examination and diagnostic tools such as an ultrasound, they can determine the cause, degree, and extent of varicose veins. They provide patients with options for treatment, which may include non-surgical or surgical methods. The specific type of treatment depends on the complexity of the varicose veins and the overall condition of the patient.

(image source: https://www.ithriveveins.com/treatment/diagnostic-venous-ultrasound)
Finding a Vascular Surgeon (Varicose Veins Specialist) in Singapore
The Vascular & Interventional Centre in Singapore offers minimally invasive treatment for varicose veins. Our vascular surgeons are well-trained in screening, diagnosing, and treating this condition. To find out if the procedure is right for you, you may request a consultation so you can understand your options and choose the best treatment for you. You can contact us at +65 6694 6270 during clinic hours or you can send an e-mail to en*****@***********tr.com.
Examining the Different Treatment Options for Varicose Veins
1.Non-surgical Treatment Options
Compression stockings improve blood flow within the leg veins, providing relief from associated symptoms, and impeding the progression of the condition. This can effectively boost blood circulation and alleviate discomfort. This specific treatment option may only be effective on mild cases of spider veins. It’s important to explore alternative treatment options, especially in cases of severe varicose veins.
2.Surgical Treatment Options
Traditional open surgery for varicose veins is commonly referred to as “high-tie ligation and vein stripping.” This procedure necessitates general anesthesia and typically involves an overnight hospital stay. While it has been a conventional approach, open surgery is often associated with several drawbacks. Patients undergoing this method tend to experience higher levels of postoperative pain, and the recovery process can be slower compared to more modern and minimally invasive alternatives. Generally, open surgical procedures carry increased risks and complications.
3.Minimally Invasive Procedures
Minimally invasive procedures offer similar benefits to traditional surgery but come with reduced pain and faster recovery times. These procedures involve small incisions rather than large openings. This technology allows for tiny punctures through which probes are inserted to seal the affected vein. Typically performed as day surgery, this approach allows for a swift return to daily activities without the need for a prolonged hospital stay. It is conducted under local anesthesia or light sedation, utilizing heat, mechanical, or chemical methods to seal the vein efficiently.
A. Radio Frequency Ablation (RFA) – Radiofrequency energy is used to heat up and damage the vein wall. A fast and safe outpatient procedure, it takes about 35-40 minutes to perform.
B. Venseal™/VenaBlock Glue Closure – A small amount of specially formulated medical adhesive is used to seal the varicose vein permanently. Through the closure of these veins, blood is rerouted to healthy veins located nearby, providing relief. This procedure provides a comfortable experience and typically is completed within 15-20 minutes.
C. Clarivein™ Mechanochemical Ablation – This procedure combines the mechanical destruction of the veins and the injection of sclerosant (a chemical used in sclerotherapy that seals off veins). A special catheter is inserted that has a wire rotating at high speed, damaging the innermost layer of the vein (or the venous intima). At the same time, there is the controlled injection of sclerosant which seals off the vein. This is a painless technique which requires a lot less local anaesthetic injection. Additionally, there is no risk of heat-induced to surrounding nerves due to the mechanochemical ablation technique.
D. Cryo-Laser and Cryo-Sclerotherapy (CLaCs) – Suitable for spider veins, this procedure combines transdermal laser and injection sclerotherapy using a chemical sclerosant, all under skin cool (-20C). It leaves minimal scarring and pigmentation post-surgery. This procedure makes use of the Harmony XL PRO. Using its light, laser, and AFT (Advanced Fluorescence Technology), affected blood vessels beneath the skin are targeted.
How to Maintain Results After Varicose Vein Treatment
While undergoing treatment from a vascular surgeon can bring relief from the pain, swelling, and cosmetic concerns associated with varicose veins, it’s equally important to recognize the significance of follow-up check-ups with these specialized medical professionals.
After successful varicose vein treatment, the initial results are often gratifying. Pain diminishes, swelling subsides, and the appearance of veins improves. However, the nature of varicose veins means that they can return, or new ones may develop over time. This is why regular check-ups with a vascular surgeon are highly recommended.
Vascular surgeons possess the expertise to monitor your vascular health and detect any potential issues early on. They can evaluate the effectiveness of the initial treatment, identify new problem areas, and recommend appropriate measures to maintain the results achieved. Patients should also follow any guidelines or instructions provided by their vascular surgeon for post-treatment care.
FAQs:
Varicose veins are primarily caused by weakened or damaged valves in the veins, leading to blood pooling and the veins becoming swollen and twisted.
Various treatments for varicose veins include minimally invasive procedures like Radio Frequency Ablation, Venseal™/VenaBlock Glue Closure, Clarivein™ Mechanochemical Ablation, Cryo-Laser and Cryo-Sclerotherapy (CLaCs), as well as traditional vein stripping surgery.
During varicose vein treatment, you can expect to be in a clinic or medical centre setting. Minimally invasive procedures often involve local anesthesia, and the surgeon will use ultrasound guidance to treat the affected veins. After treatment, you’ll typically wear compression stockings and follow post-procedure instructions for a smooth recovery.
The time it takes to see results from varicose vein treatment can vary depending on the type of treatment and the individual. In many cases, initial improvements in symptoms and appearance can be noticeable within a few weeks to a couple of months.
To maintain the results of varicose vein treatment, it’s essential to follow your vascular surgeon’s recommendations, which may include wearing compression stockings, engaging in regular physical activity, maintaining a healthy weight, and attending follow-up appointments for monitoring and preventive care. These measures help reduce the risk of varicose veins returning.
References:
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/varicose-veins-and-spider-veins
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/varicose-veins
- https://my.clevelandclinic.org/health/diseases/23331-varicose-veins-in-pregnancy
- https://www.sgvascularctr.com/service/vein-diseases-varicose-veins/

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- Treatment of varicose veins
- Treatment of varicose veins Singapore
- varicose vein specialist Singapore
- Varicose veins
- Varicose Veins Doctor Singapore
- Varicose veins in legs Singapore
- Varicose veins pregnancy Singapore
- varicose veins procedure singapore
- Varicose Veins Singapore
- Varicose veins surgery
- Varicose veins surgery Singapore
- varicose veins treatment
- varicose veins treatment singapore
